Living with COPD can be challenging, as the symptoms often cause shortness of breath, fatigue, and anxiety. In this article, we will explore various tips and techniques to help you find calm and relief from the symptoms of COPD. Whether it’s through deep breathing exercises, relaxation techniques, or making necessary lifestyle changes, we’ve got you covered. So, if you’re looking for ways to calm down and improve your quality of life with COPD, keep reading.

Understanding COPD
Overview of COPD
COPD, or chronic obstructive pulmonary disease, is a chronic respiratory disease that affects millions of people worldwide. It is a progressive condition that causes airflow obstruction in the lungs, making it difficult to breathe. COPD is characterized by chronic bronchitis and emphysema, which can lead to symptoms such as coughing, wheezing, shortness of breath, and chest tightness. It is important to understand COPD and its impact on your health in order to effectively manage this condition.
Causes of COPD
The primary cause of COPD is tobacco smoking, with about 90% of cases attributed to this harmful habit. However, long-term exposure to other lung irritants such as air pollution, secondhand smoke, and occupational hazards can also contribute to the development of COPD. Genetic factors, such as alpha-1 antitrypsin deficiency, can also increase the risk of developing COPD. It is essential to identify and address the underlying causes of COPD to prevent further progression of the disease.
Symptoms of COPD
COPD can manifest in various symptoms that can significantly impact your daily life. Some common symptoms include chronic cough, often accompanied by mucus production, shortness of breath, especially during physical activity, wheezing, and chest tightness. These symptoms may worsen over time, leading to frequent respiratory infections, weight loss, and fatigue. If you experience any of these symptoms, it is important to consult with your healthcare provider for a proper diagnosis and treatment plan.
Medical Treatment Options
Bronchodilators
Bronchodilators are medications that relax the bronchial muscles and widen the airways, making breathing easier for individuals with COPD. These medications are available in various forms, including inhalers, nebulizers, and oral tablets. Short-acting bronchodilators provide quick relief for acute symptoms, while long-acting bronchodilators help manage symptoms over a longer period of time. Bronchodilators are a cornerstone of COPD treatment and should be used as prescribed by your healthcare provider.
Inhaled steroids
Inhaled steroids, also known as corticosteroids, help reduce airway inflammation and prevent exacerbations in individuals with COPD. These medications are typically prescribed for individuals with moderate to severe COPD who continue to experience symptoms despite bronchodilator use. Inhaled steroids can be used in combination with bronchodilators to provide optimal symptom control. It is important to use inhaled steroids exactly as prescribed and to regularly monitor for potential side effects.
Oral medications
In addition to bronchodilators and inhaled steroids, oral medications may be prescribed to manage COPD symptoms. These medications, such as phosphodiesterase-4 inhibitors and oral steroids, work by reducing inflammation in the airways and improving lung function. Oral medications are typically prescribed for individuals with severe COPD or those who have frequent exacerbations. It is important to follow the prescribed dosage and discuss any potential side effects with your healthcare provider.
Oxygen therapy
For individuals with severe COPD who have low levels of oxygen in their blood, oxygen therapy may be recommended. Oxygen therapy involves the use of supplemental oxygen to improve oxygen levels and relieve symptoms of breathlessness. This can be administered through a nasal cannula or a mask, depending on individual needs. Oxygen therapy can significantly improve quality of life and overall health for individuals with severe COPD.
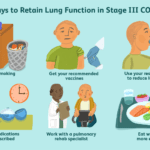
Pulmonary rehabilitation
Pulmonary rehabilitation is a comprehensive program that combines exercise training, breathing exercises, education, and emotional support for individuals with COPD. This program aims to improve lung function, reduce symptoms, and enhance overall physical and emotional well-being. Pulmonary rehabilitation is usually conducted under the guidance of healthcare professionals, such as respiratory therapists and physiotherapists. Engaging in pulmonary rehabilitation can greatly improve your ability to manage COPD and lead a fulfilling life.
Lifestyle Changes
Quitting smoking
If you are a smoker with COPD, quitting smoking is the most important step you can take to improve your health and slow down the progression of the disease. Smoking cessation plays a crucial role in reducing symptoms, preventing further lung damage, and improving overall lung function. There are many resources available to help you quit smoking, including nicotine replacement therapy, medications, and support groups. Talk to your healthcare provider about developing a personalized plan to quit smoking and kick the habit for good.
Avoiding triggers and irritants
Identifying and avoiding triggers and irritants that worsen your COPD symptoms is essential for managing the condition. Common triggers include exposure to smoke, air pollution, fumes, dust, and certain chemicals. Take steps to minimize your exposure to these irritants by using air purifiers, wearing masks when necessary, and avoiding environments with poor air quality. Making your home and workplace COPD-friendly can significantly reduce symptoms and improve your quality of life.
Maintaining a healthy weight
Maintaining a healthy weight is important for individuals with COPD as being overweight or underweight can worsen symptoms and lung function. Speak to a healthcare provider or a registered dietitian to develop a personalized nutrition plan that promotes a healthy weight. Eating a balanced diet rich in fruits, vegetables, whole grains, and lean protein can help support your respiratory health and overall well-being.
Eating a balanced diet
A balanced diet is important for individuals with COPD as it provides essential nutrients that support lung health and overall immune function. Aim to include foods that are rich in antioxidants, such as fruits and vegetables, as they help reduce inflammation in the airways. Omega-3 fatty acids found in fatty fish, nuts, and seeds can also have anti-inflammatory effects and promote lung health. Consult with a healthcare provider or a registered dietitian to develop a personalized diet plan that meets your specific nutritional needs.
Staying physically active
Regular physical activity is beneficial for individuals with COPD as it can improve lung function, reduce breathlessness, and enhance overall endurance. Engage in activities such as walking, cycling, swimming, and strength training, as they can strengthen the respiratory muscles and improve cardiovascular fitness. Start with low-impact exercises and gradually increase the intensity as tolerated. It is important to consult with your healthcare provider before initiating any exercise program to ensure it is suitable for your individual needs.
Breathing Techniques
Pursed lip breathing
Pursed lip breathing is a breathing technique that can help improve lung function and reduce breathlessness in individuals with COPD. It involves inhaling slowly through the nose and exhaling gently through pursed lips, as if blowing out a candle. Pursed lip breathing helps regulate breathing patterns, reduces air trapping in the lungs, and improves overall ventilation. Practice this technique regularly to enhance your ability to manage breathlessness during daily activities.
Diaphragmatic breathing
Diaphragmatic breathing, also known as belly breathing or abdominal breathing, involves deep inhalation and exhalation using the diaphragm muscle. This technique helps improve the efficiency of breathing, strengthens the diaphragm, and reduces respiratory effort. To practice diaphragmatic breathing, place one hand on your abdomen and inhale deeply through your nose, allowing your abdomen to rise. Exhale slowly through pursed lips, allowing your abdomen to fall. Repeat this exercise several times a day to enhance your respiratory function.
Controlled coughing
Coughing is a natural reflex that helps clear mucus and irritants from the airways. However, individuals with COPD may have a weakened cough reflex, making it difficult to clear excessive mucus. Controlled coughing can help improve mucus clearance and reduce the risk of respiratory infections. To perform controlled coughing, take a deep breath, hold it briefly, and then cough forcefully while leaning forward slightly. This technique helps generate enough force to clear mucus without straining the lungs.
Using a handheld fan
Using a handheld fan can provide temporary relief from breathlessness and help regulate breathing during episodes of increased symptoms. Hold the fan in front of your face and exhale slowly into the airflow. This technique helps create a backpressure in the airways, preventing them from collapsing and facilitating easier breathing. Carry a handheld fan with you for quick and convenient relief whenever you experience breathlessness.

Relaxation Techniques
Deep breathing exercises
Deep breathing exercises, also known as belly breathing or diaphragmatic breathing, help promote relaxation and relieve stress and anxiety. Sit or lie down in a comfortable position and place one hand on your abdomen. Inhale deeply through your nose, allowing your abdomen to rise, and exhale slowly through pursed lips, allowing your abdomen to fall. Focus on the sensation of your breath and let go of any tension or worries. Deep breathing exercises can be practiced anytime, anywhere, and can be a valuable tool for managing stress.
Progressive muscle relaxation
Progressive muscle relaxation is a technique that involves tensing and then releasing different muscle groups in the body to promote relaxation and reduce muscle tension. Start by tensing the muscles in your toes and feet, hold for a few seconds, and then release. Move upward to the calves, thighs, abdomen, shoulders, and so on, tensing and releasing each muscle group. This technique helps increase body awareness, relieve physical tension, and promote overall relaxation.
Guided imagery
Guided imagery is a relaxation technique that involves using your imagination to create a calm and peaceful environment. Close your eyes and visualize a serene place, such as a beach or a lush forest. Engage all your senses and immerse yourself in the details of this imagined environment. Take deep breaths and allow yourself to fully experience the tranquility and relaxation that this mental imagery provides. Guided imagery can be practiced individually or with the guidance of a meditation app or audio recording.
Yoga and meditation
Yoga and meditation are holistic practices that combine physical postures, breathing techniques, and mindfulness to promote relaxation and overall well-being. Yoga focuses on gentle stretching and strengthening exercises, while meditation involves cultivating a focused and present state of mind. Practicing yoga and meditation regularly can help reduce stress, improve lung function, and enhance self-awareness. Joining a yoga or meditation class can provide guidance and support in incorporating these practices into your daily routine.
Avoiding Respiratory Infections
Washing hands regularly
Proper hand hygiene is crucial for preventing respiratory infections, especially for individuals with COPD who may have a weakened immune system. Wash your hands thoroughly with soap and water for at least 20 seconds, especially before eating, after using the restroom, and after being in public spaces. If soap and water are not available, use alcohol-based hand sanitizers to effectively kill germs and reduce the risk of infection.
Getting vaccinated
Vaccinations, such as the influenza (flu) vaccine and the pneumococcal vaccine, are essential for individuals with COPD to prevent respiratory infections. The flu vaccine helps protect against strains of influenza that can cause severe illness, while the pneumococcal vaccine guards against certain bacteria that can lead to pneumonia and other pneumococcal infections. Consult your healthcare provider to ensure you are up to date with all recommended vaccinations for individuals with COPD.
Avoiding close contact with sick individuals
Close contact with individuals who have respiratory infections, such as the common cold or the flu, increases the risk of contracting these illnesses. Limit your exposure to sick individuals by avoiding crowded places, especially during peak flu seasons. If necessary, wear a mask to protect yourself from respiratory droplets that may contain infectious particles. Practicing good respiratory hygiene, such as covering your mouth and nose when coughing or sneezing, can also help prevent the spread of respiratory infections.
Using a mask in crowded places
In situations where maintaining physical distance from others is challenging, wearing a mask can provide an extra layer of protection against respiratory infections. Masks, particularly those with a high-filtration efficiency such as N95 respirators, can help filter out infectious particles in the air. Ensure that the mask fits snugly over your nose and mouth, and follow proper mask-wearing and hygiene practices. Wearing a mask is especially important during flu seasons or when you are experiencing increased COPD symptoms.
Managing Anxiety and Stress
Identifying triggers
Identifying the triggers that contribute to your anxiety and stress is an important first step in managing these emotions effectively. Common triggers may include COPD symptoms, medical appointments, financial concerns, or social situations. Pay attention to your thoughts and emotions surrounding these triggers and work towards developing coping mechanisms to address them.
Practicing relaxation techniques
Relaxation techniques, such as deep breathing exercises and progressive muscle relaxation, can help calm your mind and reduce anxiety and stress. Set aside dedicated time each day to practice these techniques and cultivate a sense of calm and peace. Experiment with different relaxation techniques to find the ones that work best for you, and incorporate them into your daily routine.
Seeking support from loved ones
Seeking support from your loved ones can greatly alleviate anxiety and stress associated with COPD. Share your concerns, fears, and challenges with trusted family members and friends who can provide empathy, understanding, and encouragement. Having a support network can reduce feelings of isolation and help you navigate the emotional ups and downs of living with COPD.
Consulting a mental health professional
If anxiety and stress become overwhelming or interfere with your daily life, consider consulting a mental health professional, such as a therapist or counselor. These professionals can provide valuable support, guidance, and coping strategies specific to your individual needs. Mental health professionals can help you develop healthy ways of managing anxiety and stress and improve your overall emotional well-being.
Palliative Care and Support
Understanding palliative care
Palliative care is a specialized medical approach that focuses on providing relief from the symptoms, pain, and stress of a serious illness, such as COPD. It is intended to improve the quality of life for individuals with chronic illnesses and their families. Palliative care is provided by a team of healthcare professionals who collaborate to address physical, emotional, and spiritual needs. Understanding the role of palliative care and discussing it with your healthcare provider can help you make informed decisions about your care.
Hospice care
Hospice care is a form of palliative care that is specifically provided to individuals who have a life-limiting illness and are no longer seeking curative treatment. Hospice care focuses on providing comfort and support during the end-of-life stage. It is a comprehensive approach that addresses not only physical symptoms but also emotional, social, and spiritual aspects. Hospice care can be provided in various settings, including home, assisted living facilities, or specialized hospice centers.
Support groups
Joining a support group can be immensely beneficial for individuals with COPD, as it provides a safe space to share experiences, receive emotional support, and learn coping strategies from others facing similar challenges. Support groups can be local, in-person gatherings or virtual communities where individuals connect online. Hearing from others who have successfully managed COPD and learning from their experiences can help you feel supported and empowered.
Talking to a counselor
Speaking with a counselor or mental health professional can provide valuable emotional support and guidance for individuals with COPD. A counselor can help you navigate the complex emotions associated with living with a chronic illness, manage anxiety and depression, and develop coping strategies. Counseling can be a safe and confidential space to explore your thoughts and feelings surrounding COPD and its impact on your life.
Healthy Sleeping Habits
Maintaining a consistent sleep schedule
Establishing a consistent sleep schedule is important for individuals with COPD to ensure adequate rest and enhance overall well-being. Aim to go to bed and wake up at the same time every day, even on weekends, to regulate your body’s internal clock. Creating a routine around sleep can help signal to your body that it is time to wind down and promote more restful sleep.
Creating a relaxing bedtime routine
Engaging in a relaxing bedtime routine can help prepare your body and mind for sleep. Establish a routine that suits your preferences and incorporates activities that promote relaxation, such as taking a warm bath, reading a book, or practicing relaxation techniques. Avoid stimulating activities or exposure to bright screens close to bedtime, as they can interfere with sleep quality.
Avoiding caffeine and heavy meals before bedtime
Caffeine, found in beverages such as coffee, tea, and energy drinks, can interfere with sleep by stimulating the central nervous system. Avoid consuming caffeine in the afternoon and evening to prevent sleep disturbances. Additionally, heavy meals close to bedtime can cause discomfort and disrupt sleep. Opt for lighter meals in the evening and allow sufficient time for digestion before lying down.
Using a comfortable mattress and pillows
A comfortable sleep environment can greatly enhance the quality of your sleep. Invest in a good-quality mattress and pillows that provide adequate support and comfort for your body. Consider factors such as mattress firmness, pillow thickness, and proper alignment of your spine. Experiment with different sleep positions and bedding materials to find what works best for you.
Regular Check-ups and Communication
Following up with healthcare provider
Regular check-ups with your healthcare provider are crucial for monitoring your COPD, adjusting your treatment plan as needed, and addressing any concerns or questions you may have. Follow the recommended schedule for check-ups and ensure that you attend all appointments. This is an important opportunity to discuss changes in your symptoms, medication effectiveness, and any other aspects of your COPD management.
Effectively communicating symptoms
Effective communication with your healthcare provider is essential for proper management of COPD. It is important to accurately describe your symptoms, their frequency, and any changes you have noticed. Keep track of your symptoms and any triggers or patterns that you observe. This information can help your healthcare provider make informed decisions about your treatment plan and make necessary adjustments as needed.
Making necessary adjustments to treatment plan
Managing COPD is an ongoing process that may require adjustments to your treatment plan over time. Work closely with your healthcare provider to monitor the effectiveness of your current treatment regimen and make any necessary modifications. It is important to follow the prescribed medication schedule, adhere to lifestyle recommendations, and communicate openly with your healthcare provider to ensure optimal management of your COPD.
Knowing when to seek emergency help
It is important to be aware of the signs and symptoms that may require immediate medical attention. If you experience severe shortness of breath, chest pain, bluish lips or fingers, confusion, or difficulty speaking, it may indicate a medical emergency. Call emergency services or go to the nearest emergency room if you experience any of these symptoms. Prompt medical intervention is crucial in managing acute exacerbations of COPD and preventing further complications.
In conclusion, understanding COPD is essential for effectively managing this chronic respiratory condition. With a combination of medical treatment options, lifestyle changes, breathing techniques, relaxation techniques, infection prevention strategies, and emotional support, individuals with COPD can improve their quality of life and maintain better control over their symptoms. It is important to work closely with healthcare providers, make necessary lifestyle modifications, and seek appropriate support to effectively manage COPD and lead a fulfilling life.