So you’re curious about what happens at a pulmonary rehab assessment? Well, let me tell you! At a pulmonary rehab assessment, a team of healthcare professionals will assess your overall lung function and health. They will conduct various tests to gather important information about your respiratory system, such as lung capacity, oxygen levels, and exercise tolerance. These assessments are designed to provide a comprehensive understanding of your pulmonary health and to tailor a personalized rehabilitation program that best suits your needs. No need to worry though, the friendly and knowledgeable staff will guide you through every step of the assessment, ensuring your comfort and well-being throughout the process.

Initial Interview
During the initial interview, your healthcare provider will start by gathering your patient history. They will ask you about your medical background, including any previous lung conditions, surgeries, or hospitalizations. It is important to provide accurate and detailed information to help the healthcare provider develop the most effective treatment plan for you.
After collecting your patient history, your healthcare provider will conduct a symptom assessment. They will ask you questions about any respiratory symptoms you are experiencing, such as shortness of breath, coughing, or wheezing. This assessment helps the healthcare provider determine the severity of your symptoms and identify any underlying causes that may need to be addressed during your treatment.
Additionally, a lifestyle evaluation will be conducted to understand your daily routine, occupation, hobbies, and exercise habits. This evaluation helps in designing an exercise prescription that suits your lifestyle and meets your individual needs. The more information you provide, the better your healthcare provider can tailor your treatment plan to your specific circumstances.
Physical Examination
After the initial interview, your healthcare provider will move on to the physical examination. This involves measuring your vital signs, such as your blood pressure, heart rate, and oxygen saturation levels. Monitoring these indicators helps assess your overall health and provides a baseline for tracking your progress throughout the rehabilitation program.
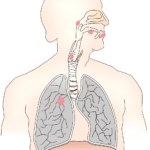
Your healthcare provider will also perform a chest auscultation, which involves listening to your lungs with a stethoscope. This examination allows them to assess your lung sounds, detecting any abnormal breath sounds that may indicate lung conditions or diseases. By identifying these abnormalities, your healthcare provider can better understand your lung function and tailor your treatment plan accordingly.
In addition to the physical examination, an exercise capacity assessment will be conducted. This involves assessing your ability to perform physical activities and gauging your exercise tolerance. By evaluating your exercise capacity, your healthcare provider can determine how well your lungs are functioning and develop an exercise plan suited to your abilities.
Lung Function Tests
To get a more comprehensive understanding of your lung health, your healthcare provider will perform lung function tests. These tests help assess various aspects of your respiratory function and provide valuable information for your treatment plan.
Spirometry is a common lung function test that measures how much air you can breathe in and out and how quickly you can exhale. It helps evaluate the amount and speed of airflow in your lungs, assisting in diagnosing and monitoring lung diseases such as chronic obstructive pulmonary disease (COPD) and asthma.
Lung volumes tests assess the amount of air in your lungs at different points in the breathing cycle. This test provides valuable information about lung diseases that affect lung volume, such as interstitial lung disease.
Diffusion capacity measures how effectively oxygen moves from your lungs into your bloodstream. This test helps evaluate the gas exchange process in your lungs and can aid in diagnosing conditions such as pulmonary fibrosis and emphysema.
By performing these lung function tests, your healthcare provider can gather objective data about your lung health, which will inform the development of your personalized treatment plan.
Exercise Prescription
Based on the information gathered during the earlier assessments, your healthcare provider will create an exercise prescription tailored to your needs and abilities. The exercise prescription aims to improve your lung function, increase your exercise capacity, and enhance your overall well-being.
The exercise goals will be determined in collaboration with you, taking into account your current fitness level and desired outcomes. Whether it’s improving endurance, reducing breathlessness, or enhancing overall physical fitness, the goals will be specific to your individual needs.
After determining the exercise goals, your healthcare provider will create an individualized plan that includes the type, duration, and intensity of exercises. This plan may include a combination of aerobic exercises, strength training, and breathing exercises designed to improve your lung function and overall fitness.
Monitoring techniques will also be implemented to track your progress throughout the program. This may involve tracking heart rate, oxygen saturation, or perceived exertion during exercise sessions. Regular monitoring helps your healthcare provider adjust your exercise program as needed and ensure you are progressing towards your goals safely and effectively.

Nutritional Assessment
A crucial component of pulmonary rehabilitation includes a nutritional assessment. Your healthcare provider will evaluate your dietary history to understand your eating habits, food preferences, and any specific dietary restrictions. This assessment helps identify any nutritional deficiencies or dietary habits that may impact your respiratory health.
Additionally, a body composition analysis may be conducted to assess your body fat percentage, muscle mass, and overall body composition. This analysis provides important information about your nutritional status and can help guide the development of a personalized nutritional plan.
Based on the assessment findings, your healthcare provider may provide nutritional counseling to address any deficiencies or imbalances in your diet. They may recommend dietary modifications, such as increasing the intake of certain nutrients or adjusting portion sizes, to optimize your overall nutrition and support your respiratory health.
Psychosocial Evaluation
Pulmonary rehabilitation also focuses on addressing the psychosocial aspects of living with a lung condition. This includes a comprehensive psychosocial evaluation to assess your mental and emotional well-being.
Depression and anxiety screening may be conducted to identify any symptoms that may be affecting your quality of life. These screenings help your healthcare provider determine if additional support or interventions are required to address any mental health challenges you may be experiencing.
A quality of life assessment may also be performed to evaluate how your lung condition impacts your overall well-being. This assessment considers factors such as your physical function, social interactions, and emotional health. By understanding how your lung condition affects your quality of life, your healthcare provider can tailor your treatment plan to address specific areas of concern.
In addition to screenings and assessments, supportive interventions may be provided. This could include referrals to mental health professionals, support groups, or counseling services. The goal is to address the psychosocial impact of your lung condition and provide you with the necessary support to improve your overall well-being.

Education and Self-Management
Education plays a vital role in pulmonary rehabilitation. It helps you understand your lung disease, its management, and how to effectively self-manage your condition. Through educational sessions, your healthcare provider will provide information and resources to empower you in managing your lung health.
The education component will cover topics such as the underlying causes of lung disease, the importance of adherence to medication regimens, and strategies for coping with breathlessness. You will also learn about proper breathing techniques to optimize lung function and reduce symptoms.
Understanding your medications and how to manage them appropriately is crucial in effectively managing your lung disease. Your healthcare provider will provide guidance on medication administration, potential side effects, and the importance of adherence to prescribed treatments.
Breathing techniques, such as pursed lip breathing and diaphragmatic breathing, will be taught to help you manage breathlessness and improve your lung function. These techniques focus on slowing down your breathing and maximizing the efficiency of oxygen exchange in your lungs.
By providing comprehensive education, your healthcare provider empowers you to take an active role in managing your lung disease and optimizing your treatment outcomes.
Smoking Cessation
As smoking is a significant risk factor for many lung diseases, smoking cessation is a crucial component of pulmonary rehabilitation. Your healthcare provider will assess your tobacco use and provide support and resources to help you quit smoking.
Assessing tobacco use involves understanding your smoking history, including the quantity and duration of smoking. This information helps your healthcare provider develop an effective smoking cessation plan that suits your needs.
Behavioral support plays a vital role in smoking cessation. Your healthcare provider may offer counseling sessions to help you address the psychological and behavioral aspects of quitting smoking. They can provide strategies, tips, and motivational support to increase your chances of successfully quitting.
Pharmacological options may also be considered to assist with smoking cessation. Your healthcare provider may recommend nicotine replacement therapy or medications that aid in reducing nicotine cravings and withdrawal symptoms. These options can be discussed and prescribed during your pulmonary rehabilitation program.
Continuum of Care
Pulmonary rehabilitation strives to provide comprehensive care that extends beyond the rehabilitation program itself. The continuum of care involves coordinating with your healthcare providers to ensure a seamless transition and continuity of care.
Your healthcare provider will communicate and collaborate with your primary care physician, pulmonologist, or other specialists involved in your lung disease management. This coordination ensures that everyone is on the same page regarding your treatment plan and goals.
Follow-up assessments will be conducted after the completion of your pulmonary rehabilitation program. These assessments help monitor your progress, address any ongoing concerns, and make any necessary adjustments to your treatment plan.
Additionally, your healthcare provider will help facilitate your transition to community programs and resources that can support your continued rehabilitation and maintenance of lung health. This may involve connecting you with local support groups, exercise programs, or educational resources to further enhance your well-being.
Individualized Treatment Plan
Based on the assessments and evaluations conducted during your pulmonary rehabilitation assessment, your healthcare provider will develop an individualized treatment plan.
The program duration will vary depending on your specific needs and goals. It may range from a few weeks to several months, with regular sessions scheduled throughout the duration of the program.
The frequency of sessions will also be determined based on your individual requirements. Typically, pulmonary rehabilitation programs involve multiple sessions per week to provide consistent support and guidance.
Reassessment criteria will be established to determine the effectiveness of the treatment plan and evaluate your progress. These criteria may include improvements in lung function, exercise tolerance, symptom management, and overall quality of life. By regularly reassessing your progress, your healthcare provider can make any necessary adjustments to optimize your treatment outcomes.
In conclusion, a comprehensive pulmonary rehabilitation assessment includes various components that help your healthcare provider understand your lung condition, determine your individual needs, and develop a personalized treatment plan. From patient history to education and self-management, the assessment aims to address all aspects of your lung health to optimize your overall well-being. Through collaboration, support, and ongoing care, pulmonary rehabilitation empowers you to take control of your lung health and improve your quality of life.