Are you struggling with chronic cough and seeking effective ways to manage it? Look no further, as this article will provide you with invaluable insights on the best practices for chronic cough management. Whether your cough is a symptom of a respiratory condition or a side effect of medication, we’ve got you covered. From lifestyle changes to medication options and home remedies, we will explore a comprehensive range of strategies that can help alleviate your cough and improve your quality of life. So bid farewell to incessant coughing and read on to discover the best practices for chronic cough management.
Diagnosis of Chronic Cough
Thorough medical history
Diagnosing the underlying cause of chronic cough requires a comprehensive medical history. Your healthcare provider will ask you questions about the duration and frequency of your cough, as well as any associated symptoms such as difficulty breathing or chest pain. They will also inquire about your medical conditions, any medications you are taking, and your lifestyle habits. It is important to provide accurate and detailed information to help your healthcare provider determine the most likely cause of your chronic cough.
Physical examination
A physical examination is an essential step in the diagnosis of chronic cough. Your healthcare provider will listen to your lungs and examine your throat and chest to check for any abnormalities or signs of respiratory conditions. They may also perform tests such as percussion, where they gently tap your chest to assess for any underlying lung conditions. Through a physical examination, your healthcare provider can gather important clues to guide further investigations and develop an appropriate management plan.
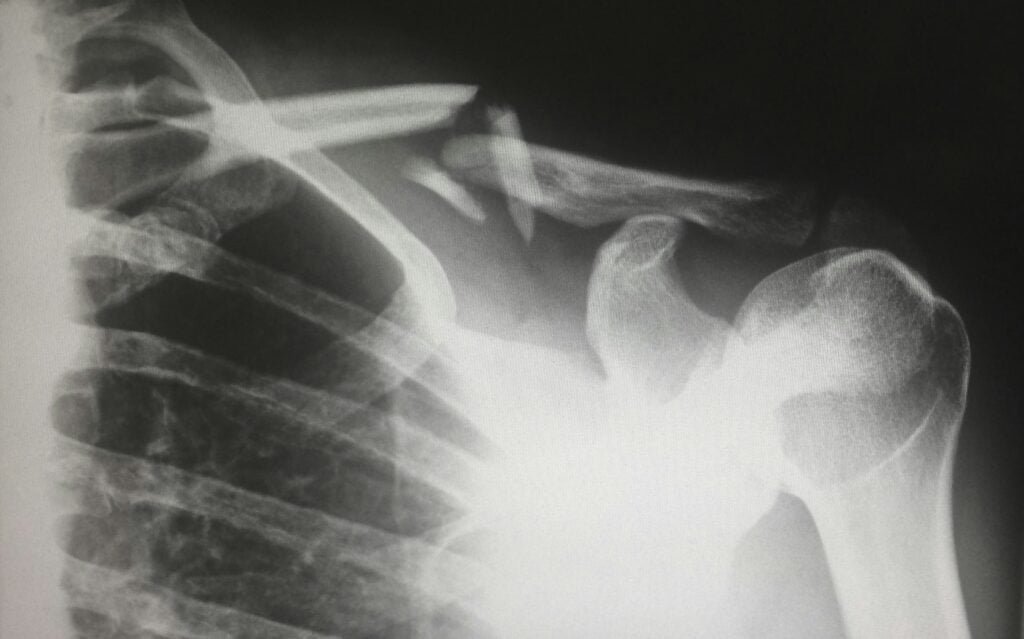
Use of diagnostic tests
In some cases, further diagnostic tests may be necessary to identify the underlying cause of chronic cough. These tests can help provide objective evidence to support the diagnosis and guide appropriate treatment. Diagnostic tests may include imaging studies such as chest X-rays or CT scans to assess the structure and function of the respiratory system. Your healthcare provider may also request pulmonary function tests to assess lung capacity and airflow. Other tests, such as allergy testing or pH monitoring for gastroesophageal reflux disease (GERD), may also be conducted to gather more information about the potential triggers for your chronic cough.
Identification and Management of Underlying Causes
Assessment for respiratory conditions
Respiratory conditions, such as asthma, chronic obstructive pulmonary disease (COPD), or bronchiectasis, can often contribute to chronic cough. Your healthcare provider will assess your symptoms, conduct breathing tests, and evaluate the results of any imaging studies to determine if a respiratory condition is contributing to your cough. If a respiratory condition is identified, specific medications and treatments targeted to that condition will be recommended to manage your chronic cough effectively.
Evaluation for gastroesophageal reflux disease (GERD)
GERD, a condition in which stomach acid flows back into the esophagus, can also be a potential cause of chronic cough. Evaluation for GERD involves assessing for common symptoms such as heartburn, regurgitation, or a sour taste in the mouth. Your healthcare provider may recommend tests such as esophageal pH monitoring or endoscopy to confirm the presence of GERD. If GERD is identified as a contributing factor to your chronic cough, lifestyle modifications, such as avoiding triggers and elevating the head of your bed, along with medications to reduce acid production, may be recommended.
Screening for medication-induced cough
Certain medications, such as angiotensin-converting enzyme (ACE) inhibitors used to treat high blood pressure, can cause a chronic cough as a side effect. It is important to inform your healthcare provider about all the medications you are taking, including over-the-counter drugs, as part of the diagnostic process for chronic cough. If a medication-induced cough is suspected, your healthcare provider may recommend discontinuing or adjusting the dosage of the medication under close supervision.
Investigation of other possible causes
While respiratory conditions and GERD are common causes of chronic cough, there are other potential underlying causes that need to be investigated. These can include nasal and sinus problems, such as allergies or chronic sinusitis, or even less common conditions like lung cancer or interstitial lung diseases. Your healthcare provider may refer you to specialists, such as allergists, pulmonologists, or otolaryngologists, to further investigate and manage these potential causes and ensure comprehensive care for your chronic cough.

Treatment of Underlying Causes
Specific medications for respiratory conditions
If your chronic cough is caused by a respiratory condition such as asthma or COPD, specific medications targeted to these conditions will be prescribed. These may include bronchodilators to help open up the airways, inhaled corticosteroids to reduce inflammation, or combination medications that address both inflammation and bronchoconstriction. It is important to follow your healthcare provider’s instructions and take these medications as prescribed to effectively manage and control your chronic cough.
Lifestyle modifications for GERD
In the case of chronic cough caused by GERD, lifestyle modifications play a crucial role in managing the condition. Your healthcare provider may recommend dietary changes, such as avoiding trigger foods or eating smaller, more frequent meals. Elevating the head of the bed while sleeping and avoiding lying down immediately after meals may also help reduce reflux and alleviate the chronic cough. In addition to lifestyle modifications, medications to reduce acid production, such as proton pump inhibitors or H2 blockers, may be prescribed to control GERD and improve your cough symptoms.
Adjustment of medications causing cough
If a medication-induced cough is identified as the cause of your chronic cough, your healthcare provider may recommend adjusting or changing the medication. It is important to discuss any concerns or potential side effects with your healthcare provider before making any changes to your medication regimen. They can guide you through the process and work with you to find alternative medications that will effectively manage your health condition while minimizing the risk of a cough.
Non-Pharmacological Therapies
Cough suppression techniques
In some cases, cough suppression techniques can help individuals with chronic cough achieve temporary relief. These techniques aim to reduce the frequency and intensity of coughing episodes. Examples of cough suppression techniques include breath control exercises, such as slow, deep breathing, or controlled coughing. Your healthcare provider or a respiratory therapist can guide you in performing these techniques effectively to minimize the impact of chronic cough on your daily life.
Breathing exercises
Breathing exercises can be beneficial for individuals with chronic cough, particularly if the cough is related to respiratory conditions such as asthma or COPD. These exercises focus on improving lung function, increasing oxygen levels, and reducing breathlessness. Examples of breathing exercises include pursed lip breathing, diaphragmatic breathing, or inspiratory muscle training. Your healthcare provider or a respiratory therapist can provide guidance on the specific breathing exercises that are most appropriate for your condition.
Airway clearance techniques
Airway clearance techniques can be helpful for individuals with chronic cough caused by conditions such as bronchiectasis or cystic fibrosis. These techniques aim to eliminate excess mucus or secretions from the airways, reducing cough and improving overall lung function. Examples of airway clearance techniques include chest physiotherapy, postural drainage, and using devices such as oscillating positive expiratory pressure devices or high-frequency chest wall oscillation vests. Your healthcare provider or a respiratory therapist can recommend and teach you the appropriate airway clearance techniques for your specific condition.
Pharmacological Therapies
Antitussive medications
Antitussive medications are drugs specifically designed to suppress coughing. These medications can be useful in managing chronic cough, particularly when other treatments have not provided sufficient relief. There are different types of antitussive medications available, including opioid and non-opioid options. However, it is important to note that these medications should be used under the guidance of a healthcare professional, as they can have potential side effects and should not be used for an extended period without medical supervision.
Inhaled corticosteroids
Inhaled corticosteroids are commonly used in the management of respiratory conditions such as asthma and COPD. These medications help reduce inflammation in the airways, alleviating symptoms such as coughing and breathlessness. In the context of chronic cough, inhaled corticosteroids may be prescribed as part of the treatment plan for underlying respiratory conditions contributing to the cough. It is important to use inhaled corticosteroids as instructed by your healthcare provider to achieve optimal control of your chronic cough.
Bronchodilators
Bronchodilators are medications that help relax and widen the airways, making it easier to breathe and reducing coughing episodes. These medications can be helpful in managing chronic cough caused by conditions such as asthma or COPD. There are different types of bronchodilators available, including short-acting or long-acting options, depending on the severity of your symptoms and the recommended treatment plan. Your healthcare provider can determine the most appropriate type of bronchodilator for your specific condition and prescribe it accordingly.
Cough Reflex Sensitivity Testing
Quantitative measurement of cough sensitivity
Cough reflex sensitivity testing involves assessing the sensitivity of your cough reflex. This test can help determine whether your cough reflex is heightened, leading to an increased frequency and intensity of coughing episodes. During the test, you may be exposed to certain irritants or stimuli, such as capsaicin or citric acid, and your cough response will be measured and compared to established norms. This quantitative measurement provides valuable information about the nature of your chronic cough and can guide treatment decisions.
Identification of hyperresponsiveness
Hyperresponsiveness refers to an exaggerated response of the airways to certain stimuli. In the context of chronic cough, identifying hyperresponsiveness can be helpful in understanding the underlying mechanisms and selecting appropriate treatment strategies. Cough reflex sensitivity testing can help identify if hyperresponsiveness is contributing to your chronic cough, enabling your healthcare provider to tailor treatment options accordingly. By addressing the hyperresponsiveness of your airways, the frequency and severity of your coughing episodes can potentially be reduced.

Patient Education and Counseling
Explaining the condition and its management
Patient education is a vital component of managing chronic cough. Your healthcare provider will explain the underlying cause of your chronic cough, addressing any concerns or questions you may have. They will discuss the recommended treatment options, including medications, lifestyle modifications, and non-pharmacological therapies, and help you understand the importance of adhering to the treatment plan. Additionally, they will provide information about potential triggers to avoid and strategies for minimizing the impact of chronic cough on your daily life.
Addressing lifestyle modifications
Lifestyle modifications can significantly impact the management of chronic cough. Your healthcare provider will discuss specific changes that may be beneficial for your condition, such as avoiding exposure to smoke or irritants, practicing good respiratory hygiene, and optimizing your overall health through regular exercise and a balanced diet. They will work with you to develop a personalized plan, tailored to your needs and preferences, that can help reduce the frequency and severity of your chronic cough.
Providing emotional support
Dealing with a chronic cough can be challenging, both physically and emotionally. Your healthcare provider understands the impact that chronic cough can have on your quality of life and emotional well-being. They are there to provide emotional support, answer your questions, and guide you through the management process. If necessary, they may recommend support groups or referral to mental health professionals who can provide additional support during your journey to manage chronic cough effectively.
Follow-Up and Monitoring
Assessing treatment response
Regular follow-up appointments with your healthcare provider are important to evaluate your response to the prescribed treatments for your chronic cough. During these visits, your healthcare provider will assess the frequency and severity of your coughing episodes, inquire about any changes in your symptoms, and review any side effects you may be experiencing. Based on this evaluation, adjustments to your treatment plan may be made to ensure optimal management of your chronic cough.
Monitoring for side effects
Some medications or treatments for chronic cough may have potential side effects. Regular monitoring and communication with your healthcare provider are essential to recognize and manage any side effects that may arise. By closely monitoring your response to treatment and promptly addressing any side effects, your healthcare provider can help ensure that your management plan remains safe and effective.
Reevaluating the management plan as needed
Chronic cough management is a dynamic process that may require adjustments over time. As your condition evolves or new information becomes available, your healthcare provider will reevaluate your management plan and make any necessary changes. This could involve adjustments to medication dosages or types, modifications to lifestyle recommendations, or exploring additional treatment options. Regular follow-up appointments provide an opportunity to reassess your chronic cough and ensure optimal management.
Collaborative Approach
Coordinating care with multiple healthcare professionals
Chronic cough management often requires a collaborative approach involving multiple healthcare professionals. Your primary care provider may work closely with specialists such as allergists, pulmonologists, otolaryngologists, or gastroenterologists to address the different aspects of your cough and develop a comprehensive management plan. This coordinated care ensures that all potential underlying causes are considered, and treatment recommendations are tailored to your specific condition.
Communication among physicians, nurses, and specialists
Effective communication among healthcare professionals is crucial in the management of chronic cough. This collaboration allows for a multidisciplinary approach to your care, ensuring that all members of your healthcare team are aware of your progress, treatment plans, and any changes in your condition. Regular communication ensures comprehensive and coordinated care, maximizing the chances of successful management of your chronic cough.
Research and Innovation
Continued study of chronic cough
Chronic cough management is an active area of research, with ongoing studies aimed at improving our understanding of the condition and developing more effective treatment strategies. Researchers are investigating the underlying mechanisms of chronic cough, exploring potential new targets for medications, and optimizing existing therapies. By participating in research studies, individuals with chronic cough can contribute to the advancement of knowledge and potentially benefit from the latest developments in the field.
Investigation of new treatment options
Innovations in the management of chronic cough are continually being explored. Researchers are investigating new treatment options, such as novel medications, advanced diagnostic techniques, or innovative non-pharmacological therapies, with the aim of providing individuals with chronic cough more effective and personalized care. By staying informed about the latest research and working closely with your healthcare provider, you can be at the forefront of emerging treatment options and potentially benefit from promising advancements.
In conclusion, the diagnosis and management of chronic cough require a thorough medical history, physical examination, and the use of diagnostic tests. Identifying and treating the underlying causes involves assessment for respiratory conditions, evaluation for GERD, screening for medication-induced cough, and investigation of other possible causes. Treatment options include specific medications for respiratory conditions, lifestyle modifications for GERD, and adjustment of medications causing cough. Non-pharmacological therapies such as cough suppression techniques, breathing exercises, and airway clearance techniques can also be beneficial. Pharmacological therapies include antitussive medications, inhaled corticosteroids, and bronchodilators. Cough reflex sensitivity testing can help quantify cough sensitivity and identify hyperresponsiveness. Patient education and counseling play a crucial role in explaining the condition, addressing lifestyle modifications, and providing emotional support. Follow-up and monitoring help assess treatment response, monitor for side effects, and reevaluate the management plan as needed. A collaborative approach involving multiple healthcare professionals and effective communication among physicians, nurses, and specialists ensures comprehensive care. Research and innovation continue to advance our understanding and treatment options for chronic cough, providing hope for improved outcomes in the future.