Living with chronic obstructive pulmonary disease (COPD) can be challenging, as it often leads to a progressive decline in lung function. But is it possible to reverse this decline and regain lung function? In this article, we will explore the potential for improving lung function in individuals with COPD and discuss strategies that can help you breathe easier and lead a more fulfilling life. So if you’ve been wondering whether it’s possible to regain lung function with COPD, keep reading to discover the answers you’ve been seeking.
Treatment options for COPD
Medications
When it comes to managing COPD, medications play a crucial role in helping you breathe easier and reduce symptoms. There are several types of medications available, and your healthcare provider will determine which ones are best for you based on the severity of your condition.
Bronchodilators are commonly prescribed for COPD and work by relaxing the muscles around your airways, allowing them to open up and improving airflow. There are two types of bronchodilators: short-acting and long-acting. Short-acting bronchodilators provide immediate relief and are used as rescue medications during flare-ups, while long-acting bronchodilators provide sustained relief and are taken regularly to prevent symptoms.
Corticosteroids, also known as anti-inflammatory drugs, are often used in combination with bronchodilators for more severe cases of COPD. These medications help reduce inflammation in the airways, making breathing easier.
In some cases, antibiotics may be prescribed if you have a bacterial infection that is worsening your COPD symptoms. Antibiotics can help clear the infection and prevent it from causing further damage to your lungs.
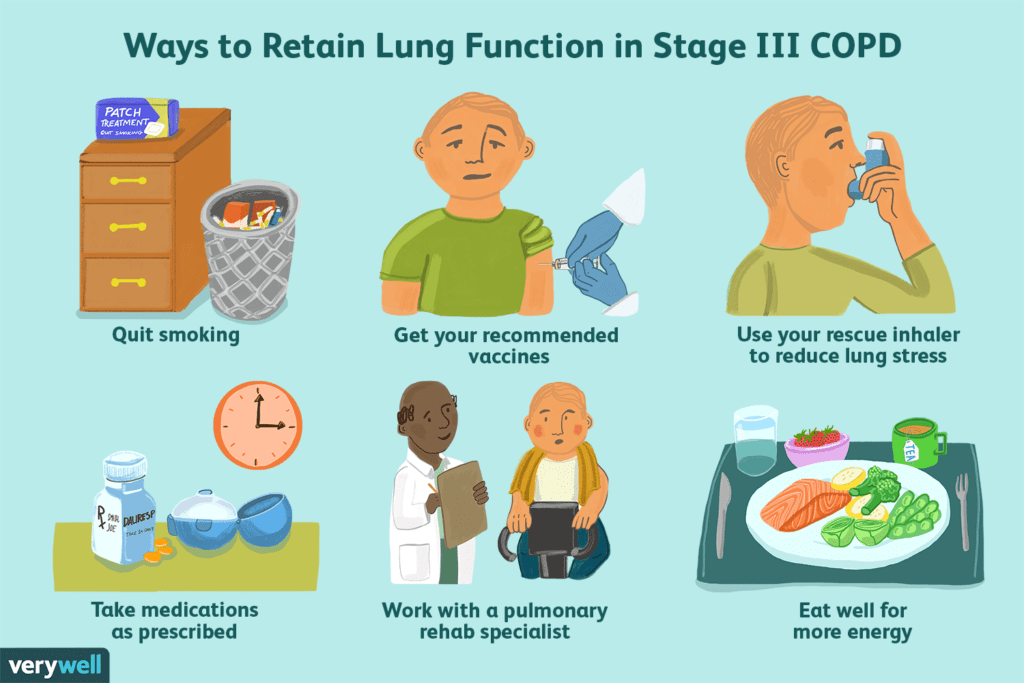
Lifestyle changes
Making certain lifestyle changes can greatly improve your quality of life with COPD. One of the most important steps you can take is to quit smoking if you are a smoker. Smoking is the leading cause of COPD, and quitting can help slow down the progression of the disease and improve lung function. It may be challenging to quit, but there are various resources available, such as smoking cessation programs and medications, that can increase your chances of success.
Another lifestyle change that can benefit those with COPD is maintaining a healthy weight. Excess weight can put additional strain on your breathing and make symptoms worse. Eating a balanced diet, exercising regularly, and working with a dietitian can help you achieve and maintain a healthy weight.
Pulmonary rehabilitation
Pulmonary rehabilitation is a comprehensive program designed to improve the overall functioning and quality of life for individuals with COPD. It involves a combination of exercise training, education, and support to help you manage your symptoms and improve your physical and emotional well-being.
During pulmonary rehabilitation, you will work closely with a team of healthcare professionals, including respiratory therapists, physiotherapists, and dietitians, who will tailor a program specifically to meet your needs. The program will typically include exercises to improve lung capacity and strength, education on managing COPD symptoms, and support for making necessary lifestyle changes.
Participating in pulmonary rehabilitation can help you regain control of your life and improve your ability to perform everyday activities. It is an essential treatment option for individuals with COPD and is highly recommended by healthcare providers.
Managing symptoms of COPD
Bronchodilators
Bronchodilators are a key component of managing COPD symptoms. These medications work by relaxing the muscles in your airways, allowing them to open up and improving airflow. By using bronchodilators, you can experience relief from symptoms such as wheezing, shortness of breath, and coughing.
There are two types of bronchodilators commonly prescribed for COPD: short-acting and long-acting. Short-acting bronchodilators provide quick relief and are often used as rescue medications during flare-ups or acute exacerbations. They work within minutes and their effects last for a few hours. Long-acting bronchodilators, on the other hand, provide sustained relief and are taken regularly to prevent symptoms and improve overall lung function.
It’s important to follow the instructions provided by your healthcare provider when using bronchodilators. They may be in the form of inhalers, nebulizers, or oral medications. Remember to always have your rescue inhaler with you in case of emergencies, and discuss any concerns or questions with your healthcare provider.
Corticosteroids
Corticosteroids, also known as glucocorticoids, are anti-inflammatory medications often used in combination with bronchodilators for more severe cases of COPD. They help reduce inflammation in your airways, making it easier to breathe.
These medications can be delivered orally, through inhalers, or intravenously, depending on the severity of your symptoms. They are typically taken for a short period during acute exacerbations or for more extended periods to manage chronic inflammation.
Corticosteroids are powerful medications that can have side effects, especially when used long-term. Common side effects include weight gain, increased blood sugar levels, and weakened immune system. It’s important to work closely with your healthcare provider to find the right balance between managing your symptoms and minimizing potential side effects.
Antibiotics
In some cases, a bacterial infection can worsen COPD symptoms and lead to exacerbations. Your healthcare provider may prescribe antibiotics to treat these infections. Antibiotics work by killing the bacteria responsible for the infection, reducing inflammation, and preventing further damage to your lungs.
It’s important to take the antibiotics exactly as prescribed, even if you start feeling better before finishing the course. This ensures that the infection is completely cleared and reduces the risk of developing antibiotic-resistant bacteria.
If you experience recurrent infections or notice a persistent change in your symptoms, it’s crucial to contact your healthcare provider. They can evaluate your condition and determine if antibiotic treatment is necessary to manage your COPD effectively.
Preventing exacerbations
Flu and pneumonia vaccines
Preventing respiratory infections is crucial for individuals with COPD. Vaccinations can help reduce the risk of contracting the flu and pneumonia, both of which can lead to a worsening of COPD symptoms and increase the risk of complications.
The flu vaccine is typically recommended annually and protects against strains of the influenza virus. It is especially important for individuals with COPD to receive the flu vaccine since they are at higher risk of developing severe complications from the flu.
Pneumonia vaccines, such as the pneumococcal conjugate vaccine (PCV13) and pneumococcal polysaccharide vaccine (PPSV23), protect against several types of the bacteria that commonly cause pneumonia. These vaccines are usually given once in a lifetime, although a booster dose of PPSV23 may be recommended for certain high-risk individuals.
Speak with your healthcare provider about when and how to receive these vaccinations. It’s important to stay up to date with immunizations to keep yourself protected and minimize the risk of exacerbations.
Avoiding irritants and triggers
Avoiding irritants and triggers that can worsen COPD symptoms is an essential aspect of managing the condition and preventing exacerbations. These irritants can include cigarette smoke, air pollution, dust, chemicals, and certain fumes.
If you are a smoker, quitting is the most effective way to improve your lung health and reduce the progression of COPD. Additionally, it’s important to avoid secondhand smoke as it can also be detrimental to your respiratory health. Avoiding places where people smoke and encouraging those around you to do the same can help create a healthy environment for your lungs.
Air pollution, both outdoor and indoor, can also be harmful to individuals with COPD. Stay informed about air quality in your area and take precautions on days when pollution levels are high.
In your home, try to eliminate or minimize exposure to dust, pet dander, and other allergens that may trigger your symptoms. Regularly clean your living space, use air filters if necessary, and ensure proper ventilation.
Regular exercise
Regular exercise is beneficial for everyone, but it is especially important for individuals with COPD. Engaging in physical activity can help improve lung capacity, increase endurance, and enhance overall well-being.
When starting an exercise program, it’s crucial to start slowly and gradually increase the intensity and duration of your workouts. Begin with low-impact activities such as walking, swimming, or cycling, and aim for at least 30 minutes of exercise most days of the week. As you become more comfortable and conditioned, you can gradually increase the intensity or try other activities such as strength training or yoga.
Consult with your healthcare provider before starting any exercise program to ensure it is appropriate for your specific needs. They can provide guidance on the types of exercises that are best for you and help you establish realistic goals.
Slowing disease progression
Smoking cessation
One of the most effective ways to slow down the progression of COPD is to quit smoking. If you are a smoker, quitting can significantly improve your lung function and overall health. It may not be easy, but there are various resources and support available to help you succeed.
Consider joining a smoking cessation program or seeking support from healthcare professionals, friends, or family members. Nicotine replacement therapy, such as patches or gum, can also be beneficial in managing withdrawal symptoms and cravings.
Every day smoke-free is a step towards improving your lung health and decreasing the progression of COPD. Stay motivated and focused on the long-term benefits of quitting.
Avoiding secondhand smoke
Even if you are not a smoker, exposure to secondhand smoke can still be detrimental to your respiratory health. Breathing in the smoke from others’ cigarettes or other tobacco products can irritate your airways and worsen COPD symptoms.
Protect yourself by avoiding places where others smoke, such as bars or designated smoking areas. If you have friends or family members who smoke, kindly ask them to refrain from smoking in your presence or in enclosed spaces.
Creating a smoke-free environment is essential for slowing down the progression of COPD and maintaining healthier lungs.
Managing comorbidities
COPD often coexists with other chronic conditions, such as cardiovascular disease, diabetes, and anxiety or depression. Managing these comorbidities is crucial in slowing down disease progression and improving overall well-being.
Work closely with your healthcare provider to develop a comprehensive treatment plan that addresses all of your health concerns. This may involve taking medications as prescribed, making lifestyle modifications, and attending regular check-ups to monitor your conditions.
By effectively managing comorbidities, you can better control your COPD symptoms and minimize the impact they have on your daily life.
Importance of exercise
Benefits of exercise for COPD
Exercise is incredibly important for individuals with COPD, as it offers a myriad of benefits for both physical and emotional well-being. Engaging in regular physical activity can significantly improve COPD symptoms and overall quality of life.
Benefits of exercise for COPD include:
Improved lung function: Exercise helps strengthen the muscles used for breathing and can increase lung capacity, allowing for more efficient airflow in and out of the lungs.
Increased endurance: Regular exercise can improve cardiovascular fitness, making everyday activities, such as walking or climbing stairs, easier and less tiring.
Reduced shortness of breath: By incorporating exercise into your routine, you can train your body to become more efficient at using oxygen, resulting in less breathlessness during physical exertion.
Enhanced mood and mental well-being: Exercise releases endorphins, which are natural mood boosters. Engaging in physical activity can help reduce anxiety, depression, and stress commonly associated with COPD.
Types of exercises recommended
When it comes to exercises for COPD, it’s important to choose activities that improve cardiovascular fitness, strengthen muscles used for breathing, and promote overall endurance. Here are some types of exercises that are recommended for individuals with COPD:
Aerobic exercises: Activities such as walking, cycling, swimming, and dancing help improve cardiovascular fitness and overall endurance. Aim for at least 30 minutes of moderate-intensity aerobic exercise most days of the week. If you are just starting, begin with shorter sessions and gradually increase the duration as you build stamina.
Strength training: Incorporating strength training exercises into your routine can help strengthen the muscles used for breathing and improve overall muscle tone. Exercises like lifting weights, using resistance bands, or using weight machines at the gym can be beneficial. Start with lighter weights and gradually increase the resistance as you get stronger.
Breathing exercises: Pursed-lip breathing exercises can be particularly helpful for individuals with COPD. This involves inhaling slowly through your nose and exhaling through pursed lips as if you are blowing out a candle. This type of breathing helps to keep your airways open and promotes better oxygen exchange.
Always consult with your healthcare provider before starting any exercise program, especially if you have severe COPD. They can provide personalized recommendations and modify exercises to suit your specific needs.
Tips for starting an exercise program
Starting an exercise program can be intimidating, especially if you have COPD. Here are some tips to help you get started:
Consult with your healthcare provider: Before embarking on any exercise program, it’s important to discuss your plans with your healthcare provider. They can assess your current health status and provide guidance on the types and intensity of exercises that are suitable for you.
Start slowly and pace yourself: Begin with shorter, less intense sessions and gradually work your way up. Listen to your body and take breaks as needed. Over time, you will be able to increase the duration and intensity of your workouts.
Stay consistent: Regular exercise is key to reaping the benefits. Strive for consistency by incorporating physical activity into your daily routine. Find activities that you enjoy and are more likely to stick with in the long run.
Stay hydrated: Drink plenty of water before, during, and after exercise to stay hydrated. Proper hydration helps keep mucus thin and easier to cough up.
Use assistive devices if needed: If you require supplemental oxygen, use it as prescribed during exercise. Portable oxygen concentrators or cylinders can be used to maintain adequate oxygen levels during physical activity.
Remember, exercise is an individual journey, and it’s important to listen to your body. If you experience severe shortness of breath, chest pain, or dizziness, stop exercising and seek medical attention. Gradually increase the intensity of your workouts as your fitness improves, but always stay within your comfort zone.
Dietary considerations for COPD
Maintaining a healthy weight
Maintaining a healthy weight is essential for individuals with COPD as excess weight can make it more difficult to breathe. Being underweight, on the other hand, can weaken muscles and decrease energy levels.
To achieve and maintain a healthy weight, it’s important to focus on proper nutrition and portion control. A dietitian can help you create a personalized meal plan that meets your individual needs and accounts for any dietary restrictions or preferences you may have.
Eating a balanced diet
A balanced diet, rich in essential nutrients, is crucial for overall health and well-being, especially for individuals with COPD. Here are some dietary considerations to keep in mind:
Protein: Including an adequate amount of protein in your diet is important for maintaining muscle strength. Good sources of protein include lean meats, fish, poultry, eggs, dairy products, legumes, and nuts.
Fruits and vegetables: Aim to include a variety of fruits and vegetables in your diet, as they are excellent sources of vitamins, minerals, and antioxidants. Choose colorful, nutrient-dense options such as berries, leafy greens, citrus fruits, and cruciferous vegetables.
Whole grains: Opt for whole grains instead of refined grains to ensure you get enough fiber, vitamins, and minerals. Examples of whole grains include whole wheat, brown rice, quinoa, and oats.
Healthy fats: Include healthy fats in your diet, such as those found in avocados, nuts, seeds, and olive oil. These fats can help reduce inflammation and provide essential nutrients for your body.
Hydration: Drink enough fluids throughout the day to stay properly hydrated. Water is the best choice, but you can also include herbal teas, broths, and low-sugar beverages in your fluid intake.
Avoiding foods that worsen symptoms
Certain foods may contribute to increased mucus production or worsen COPD symptoms in some individuals. Consider avoiding or reducing the intake of the following:
Dairy products: Some people with COPD find that consuming dairy products, such as milk and cheese, can lead to increased mucus production. If you notice this association, try reducing your intake or opting for dairy alternatives.
Gas-producing foods: Foods that are known to cause gas, such as beans, lentils, broccoli, cabbage, and carbonated beverages, may cause bloating and discomfort. Experiment with your diet to identify which foods exacerbate your symptoms and adjust accordingly.
Excess sodium: Too much sodium can cause fluid retention, which can make breathing more difficult. Limit your intake of processed foods, canned goods, and foods high in sodium. Instead, opt for fresh, whole foods and use herbs and spices to add flavor to your meals.
It’s important to listen to your body and identify any specific triggers that worsen your symptoms. Keeping a food diary can be helpful in tracking your diet and symptoms, allowing you to make informed decisions about your dietary choices.
Alternative therapies for COPD
Acupuncture
Acupuncture is an ancient Chinese technique that involves the insertion of thin needles into specific points on the body. Some individuals with COPD have found acupuncture to be beneficial in managing symptoms such as shortness of breath and coughing. Although the exact mechanism behind its effectiveness is not fully understood, acupuncture is believed to stimulate the nervous system and promote relaxation.
If you are considering acupuncture as a complementary therapy for COPD, it’s important to consult with a licensed acupuncturist who is experienced in treating respiratory conditions. They can assess your individual needs and develop a treatment plan tailored to your specific symptoms.
Herbal remedies
Herbal remedies have been used for centuries to manage various health conditions, including respiratory ailments. Certain herbs and plants have shown potential in improving lung function and relieving COPD symptoms.
Some commonly used herbal remedies for COPD include:
Ginseng: Known for its adaptogenic properties, ginseng has been used in traditional medicine to support respiratory health. It may help improve lung function and increase exercise tolerance.
Mullein: Mullein is a flowering plant that has been used to soothe respiratory irritation and reduce coughing. It is often brewed into tea or inhaled as steam.
Eucalyptus: The essential oil of eucalyptus can help open up the airways and improve breathing. It can be used in steam inhalation or diluted in a carrier oil for topical application on the chest.
It’s crucial to approach herbal remedies with caution and consult with a healthcare provider before using them, as some may interact with medications or have side effects. Additionally, herbal remedies are not regulated by the FDA, so it’s important to ensure the quality and safety of the products you choose.
Pursed-lip breathing exercises
Pursed-lip breathing exercises are a simple technique that can help alleviate shortness of breath and improve breathing efficiency. This technique involves inhaling slowly through your nose and exhaling through your mouth with pursed lips, as if you are blowing out a candle.
Pursed-lip breathing helps to prolong the exhalation phase, allowing more air to be expelled from your lungs and reducing trapped air. It can also help regulate breathing patterns, slow down respiration rate, and promote relaxation.
Practice pursed-lip breathing exercises regularly, especially during physical exertion or when you feel breathless. It can be incorporated into your daily routine and used as a tool to manage breathlessness in various situations.
Surgical options for COPD
Lung volume reduction surgery
Lung volume reduction surgery (LVRS) is a surgical procedure performed to remove a portion of the damaged lung tissue. This surgery can help improve lung function, decrease breathlessness, and enhance overall quality of life for individuals with advanced COPD.
During the procedure, a surgeon removes damaged areas of the lung, allowing the remaining healthy tissue to function more efficiently. This can result in improved lung function, increased exercise tolerance, and reduced respiratory symptoms.
LVRS is typically considered for individuals with severe emphysema, a type of COPD characterized by the destruction of lung tissue. It is important to undergo a thorough evaluation to determine if you are a suitable candidate for this surgery.
Lung transplant
For individuals with end-stage COPD, a lung transplant may be a viable option. This procedure involves replacing one or both diseased lungs with healthy lungs from a donor.
Lung transplantation can significantly improve lung function and quality of life for individuals with severe COPD who have exhausted other treatment options. However, it is a complex procedure that carries risks and requires a careful evaluation process to determine suitability.
After a lung transplant, lifelong immunosuppressive medications are necessary to prevent organ rejection. Regular follow-up care and close monitoring are essential to ensure the success of the transplant and manage post-transplant complications.
Bullectomy
In some cases of severe COPD, large air spaces called bullae may form within the lungs. These bullae can compress healthy lung tissue, leading to breathing difficulties.
Bullectomy is a surgical procedure that involves removing these bullae to improve lung function. It can help alleviate symptoms such as shortness of breath and enhance overall lung capacity.
This procedure is typically reserved for individuals with specific characteristics, such as the presence of large bullae and significant respiratory distress. As with any surgical procedure, a thorough evaluation is necessary to determine if you are a suitable candidate for a bullectomy.
Discuss surgical options with your healthcare provider to determine the best course of action for your specific situation. They can provide you with detailed information, discuss potential risks and benefits, and guide you through the decision-making process.
Coping with the emotional impact of COPD
Support groups
Living with COPD can be challenging, both physically and emotionally. Joining a support group can provide a sense of community and understanding among individuals facing similar circumstances.
Support groups can offer a safe space to share experiences, discuss coping strategies, and receive emotional support. They can also provide valuable information and resources about managing COPD from individuals who have firsthand knowledge.
Consider joining local support groups in your area or participating in online communities dedicated to COPD. Connecting with others who understand your journey can provide a sense of relief and empowerment.
Counseling or therapy
COPD can have a significant impact on mental health, leading to feelings of depression, anxiety, and frustration. Seeking counseling or therapy can help you navigate the emotional challenges associated with living with a chronic respiratory condition.
A mental health professional can provide support, coping strategies, and therapeutic interventions tailored to your needs. They can help you develop healthy coping mechanisms, manage stress, and maintain a positive outlook despite the challenges of COPD.
Whether through individual counseling or group therapy, addressing your emotional well-being is essential for overall quality of life and effective COPD management.
Self-care practices
Engaging in self-care practices can help improve your emotional well-being and cope with the challenges of COPD. Take time to prioritize activities that bring you joy, reduce stress, and promote relaxation.
Some self-care practices that may benefit individuals with COPD include:
Mindfulness and meditation: Practicing mindfulness and meditation can help calm the mind and reduce stress. Dedicate a few minutes each day to sit quietly, focus on your breath, or listen to guided meditation recordings.
Hobbies and interests: Pursuing activities you enjoy can provide a sense of fulfillment and distraction from the challenges of COPD. Whether it’s reading, painting, gardening, or listening to music, find activities that bring you joy and engage your mind.
Rest and sleep: Adequate rest and quality sleep are essential for physical and emotional well-being. Establish a comfortable sleep routine, create a relaxing sleep environment, and prioritize rest when needed.
Stress management: Identify triggers of stress and develop healthy coping mechanisms. This may include practicing deep breathing exercises, engaging in relaxation techniques, or talking to a trusted friend or family member.
Remember, self-care looks different for everyone. Find what works best for you and make it a priority in your daily life.
Research and future developments
Stem cell therapy
Stem cell therapy is an area of active research for COPD treatment. This innovative approach involves using stem cells to repair damaged lung tissue and potentially regenerate healthy lung cells.
Research studies have shown promising results, with some individuals experiencing improvements in lung function, quality of life, and exercise tolerance. However, stem cell therapy for COPD is still considered experimental and is typically only available through clinical trials.
As research continues to advance, stem cell therapy may become a viable treatment option for individuals with COPD, particularly those with severe disease.
Gene therapy
Gene therapy is another emerging area of research that holds potential for treating COPD. This approach involves modifying or replacing genes to correct genetic abnormalities or enhance the body’s ability to defend against lung damage.
Researchers are exploring various gene therapy techniques, including delivering genes directly to the lungs using viruses or nanoparticles. Although gene therapy for COPD is still in the early stages of development, it offers hope for more targeted and personalized treatments in the future.
New medications in development
Scientists and pharmaceutical companies are continuously working to develop new medications to improve COPD management. These medications aim to provide more targeted relief, enhance lung function, and slow down disease progression.
Some of the areas of research include:
Anti-inflammatory drugs: Researchers are exploring new anti-inflammatory drugs that can specifically target the inflammation associated with COPD without the side effects of current medications.
Bronchodilators: Novel bronchodilators with improved efficacy and fewer side effects are being developed to provide better symptom relief and enhance lung function.
Mucus clearance agents: Medications that facilitate the clearance of mucus from the airways are being researched to improve respiratory function and reduce the risk of exacerbations.
While these medications are still being studied and tested, they represent the potential for significant advancements in COPD treatment. Stay informed about ongoing research and discuss emerging treatment options with your healthcare provider.
In conclusion, managing COPD requires a multifaceted approach that includes medications, lifestyle changes, and various therapies. By following the treatment options mentioned above, such as medications, lifestyle changes, pulmonary rehabilitation, and preventative measures, you can effectively manage your COPD symptoms, slow the progression of the disease, and enhance your overall quality of life. Remember to consult with healthcare professionals and seek support from your loved ones to ensure you receive the best care and support to manage your condition. With proper management and a positive mindset, you can regain control and live a fulfilling life with COPD.