
Whether you’re a parent, caregiver, or simply curious about child health, understanding the signs of respiratory distress in infants and children is crucial. When it comes to their well-being, it’s important to be aware of the subtle cues and symptoms that could indicate respiratory problems. From rapid breathing to wheezing and grunting, this article will shed light on the telltale signs you need to watch out for, enabling you to respond promptly and ensure the best possible care for your little ones.
Overview of Respiratory Distress
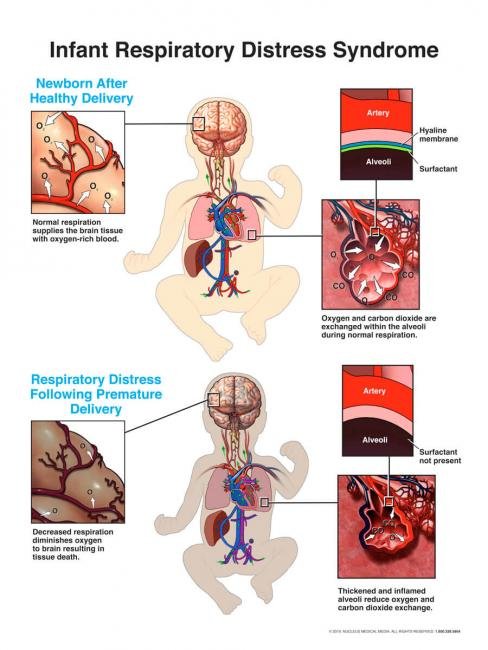
Respiratory distress refers to a condition in which there is a difficulty in breathing or inadequate oxygen intake by the body. It is crucial to recognize respiratory distress in infants and children as it can be a sign of a serious underlying medical condition. Prompt identification and treatment of respiratory distress can help prevent complications and improve outcomes.
Definition of Respiratory Distress
Respiratory distress is characterized by a range of physical and behavioral signs that indicate a respiratory problem. These signs may include rapid breathing, flaring nostrils, retractions (visible sinking of the skin between the ribs and at the base of the neck), grunting, and cyanosis (bluish discoloration of the skin and mucous membranes). Behavioral signs of respiratory distress can include irritability, restlessness, refusal to eat or drink, and excessive drowsiness.
Importance of Recognizing Respiratory Distress in Infants and Children
Recognizing respiratory distress in infants and children is crucial because it allows for early intervention and proper management. Infants and young children are more susceptible to respiratory distress due to their small airways and immature immune systems. Failure to recognize and address respiratory distress promptly can lead to severe complications, such as respiratory failure or even death. By being vigilant and acknowledging the signs of respiratory distress, caregivers can ensure the well-being of their little ones.
Common Causes of Respiratory Distress
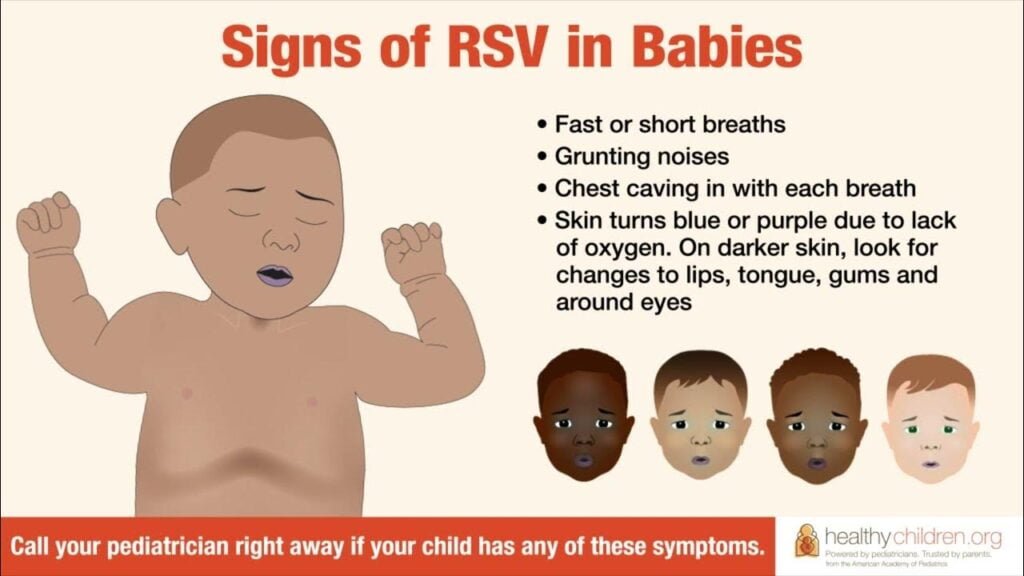
There are several common causes of respiratory distress in infants and children. Viral infections, such as the common cold or the flu, are a frequent culprit. Asthma, a chronic inflammatory disease of the airways, can also lead to respiratory distress. Pneumonia, a lung infection, is another common cause. Croup, characterized by a barking cough and difficulty breathing, affects the upper airways. Lastly, bronchiolitis, typically caused by the respiratory syncytial virus (RSV), is an inflammation of the small airways in the lungs. Recognizing these common causes can help in identifying and managing respiratory distress effectively.
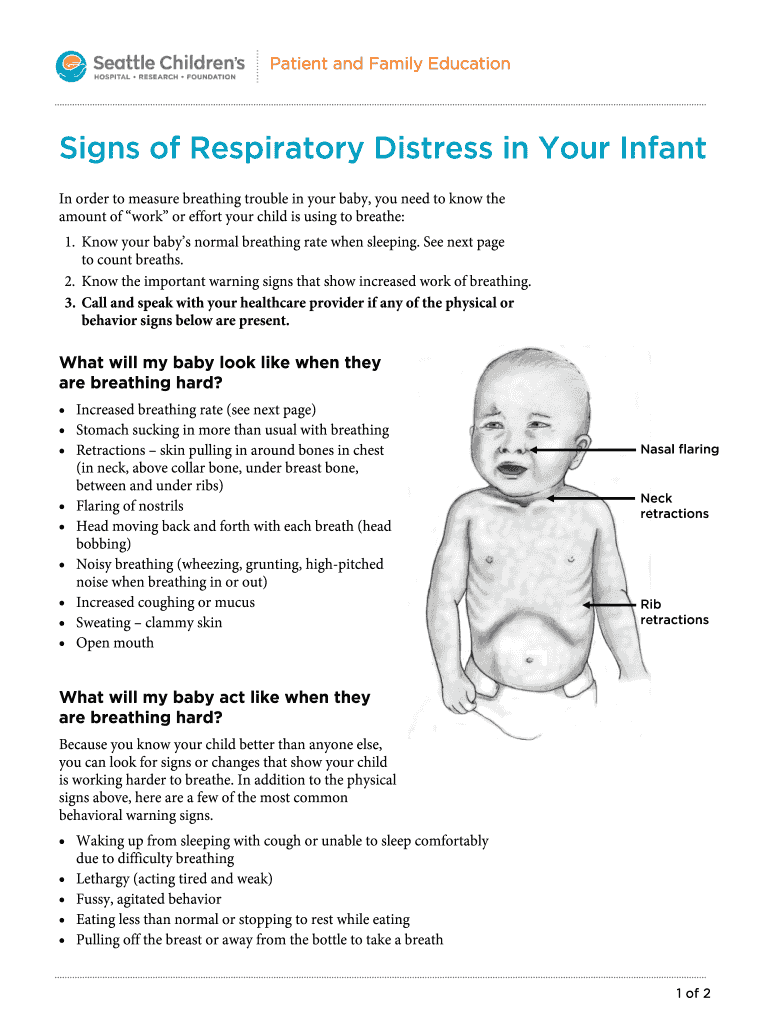
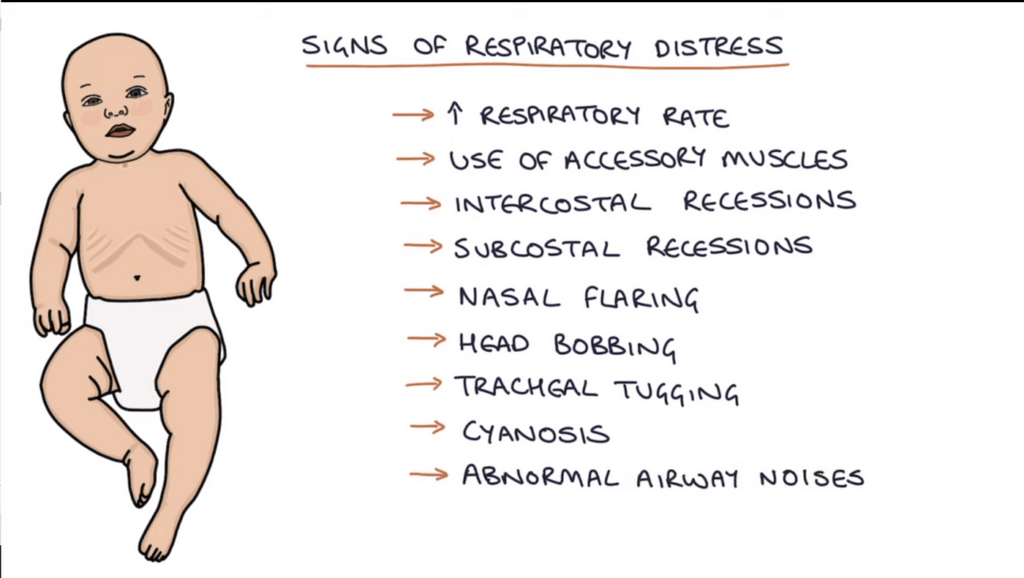
Physical Signs of Respiratory Distress
When observing a child for signs of respiratory distress, there are various physical signs to look out for. Rapid breathing, indicated by a faster than normal respiratory rate, is a common physical sign. Flaring nostrils, where the nostrils widen during breathing, can also be observed. Retractions, the visible sinking of the skin between the ribs or at the base of the neck, are another physical indication of respiratory distress. Grunting, a sound made when exhaling, as well as cyanosis, a bluish discoloration of the skin and mucous membranes, are further signs that should not be ignored.
Behavioral Signs of Respiratory Distress
Not all signs of respiratory distress are physical; there are also behavioral signs to be aware of. Irritability is one such sign, where a child may appear easily agitated or upset. Restlessness, wherein a child is unable to settle or constantly moves, can also indicate respiratory distress. A refusal to eat or drink is another behavioral sign, suggesting that the child finds it difficult to do so due to respiratory discomfort. Excessive drowsiness, where a child is abnormally sleepy or difficult to wake up, can also be a red flag for respiratory distress.
Assessment Techniques
To determine the presence and severity of respiratory distress, various assessment techniques can be used. Listening for abnormal breath sounds, such as wheezing or crackles, can provide important clues. Checking oxygen saturation levels using a pulse oximeter can help evaluate the child’s oxygen levels. Observing chest movements during breathing can reveal any abnormalities or signs of distress. Measuring the respiratory rate, either visually or with a timer, can quantify the child’s breathing pattern. Assessing the general appearance of the child, including skin color and overall behavior, can also aid in determining the severity of respiratory distress.
Emergency Actions
When faced with a child in respiratory distress, it is important to take immediate actions to ensure their safety and well-being. Seeking immediate medical attention is crucial, as healthcare professionals can provide proper assessment and treatment. If emergency medications, such as bronchodilators or epinephrine, have been prescribed, administering them as directed can help alleviate symptoms. In extreme cases where the child is not breathing or has no pulse, performing CPR (cardiopulmonary resuscitation) may be necessary to maintain circulation and deliver oxygen to the body.

Preventing Respiratory Distress
While not all cases of respiratory distress can be prevented, there are steps that can be taken to reduce the risk. Keeping infants and children up to date on their vaccinations, especially those targeting respiratory infections like influenza and pneumococcus, can help prevent certain respiratory illnesses. Maintaining good hand hygiene by regularly washing hands and avoiding close contact with individuals who are sick can also reduce the spread of respiratory infections. Additionally, avoiding exposure to smoke and pollutants, such as cigarette smoke and air pollution, is important in maintaining respiratory health. Creating a healthy environment with good indoor air quality can also contribute to preventing respiratory distress.
When to Call a Doctor
There are certain situations in which it is crucial to call a doctor when a child is experiencing respiratory distress. If the symptoms persist or worsen despite initial care at home, contacting a healthcare professional is necessary. Severe breathing difficulties, such as rapid or labored breathing, or high fever should not be ignored and must be addressed by a medical professional. Lethargy, where a child is unusually tired and unresponsive, can also be a sign of a serious problem and requires immediate medical attention.
Treatment Options
Treatment options for respiratory distress vary depending on the specific cause and severity of the condition. Medications, such as bronchodilators or corticosteroids, may be prescribed to relieve symptoms and reduce airway inflammation. Oxygen therapy, delivered through specialized equipment, can help improve oxygen levels in the blood. In severe cases, hospitalization may be required to provide additional support and monitoring, especially when a child’s condition does not respond to outpatient management or when complications arise.
Importance of Early Intervention
Early intervention in cases of respiratory distress is crucial for several reasons. By addressing respiratory distress promptly, complications can be prevented or minimized. Timely treatment can help reduce the severity and duration of symptoms, improving the child’s overall well-being. Furthermore, early intervention can lead to better outcomes, preventing the development of chronic respiratory conditions and decreasing the risk of long-term complications. By recognizing and acting upon the signs of respiratory distress in infants and children, caregivers can play a vital role in ensuring optimal respiratory health.









