Living with COPD can be challenging, but there is hope for improvement. With proper management and a proactive approach, individuals with COPD can experience a better quality of life. From implementing lifestyle changes to utilizing various treatment options, there are several ways to help alleviate symptoms and slow down the progression of the disease. While COPD may not be completely curable, it is definitely possible for individuals to achieve significant improvements in their respiratory function and overall well-being. So, if you or someone you know is dealing with COPD, rest assured that there are steps you can take to make things better.
Understanding COPD
Definition of COPD
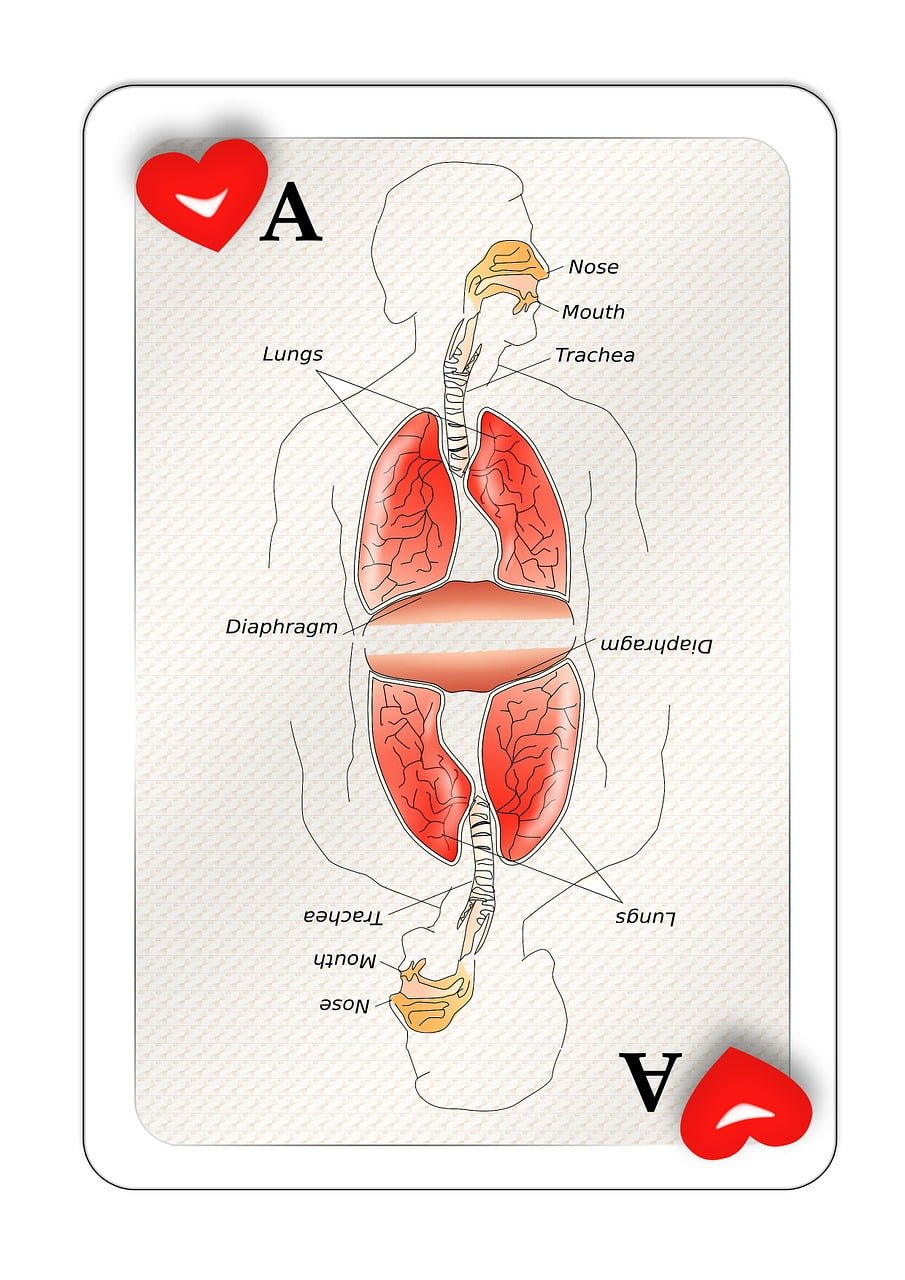
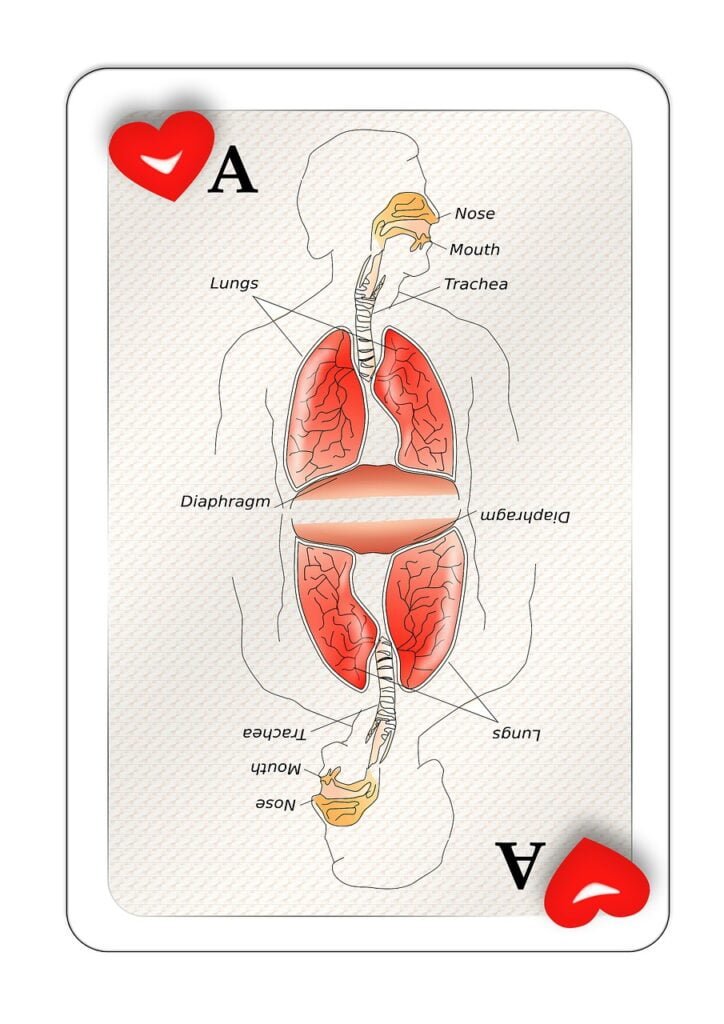
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung disease that obstructs airflow, making it difficult to breathe. It is often characterized by symptoms such as coughing, wheezing, shortness of breath, and chest tightness. COPD primarily includes two conditions – chronic bronchitis and emphysema. Chronic bronchitis involves inflammation of the bronchial tubes, leading to excessive mucus production. Emphysema refers to the damage and destruction of the air sacs in the lungs, reducing their elasticity and impairing the exchange of oxygen and carbon dioxide.
Causes of COPD
COPD is commonly caused by long-term exposure to harmful substances that irritate and damage the lungs. The most significant risk factor is tobacco smoking, accounting for nearly 90% of COPD cases. Other factors that contribute to COPD include exposure to environmental pollutants (such as fumes, chemicals, and dust), genetic predisposition (alpha-1 antitrypsin deficiency), and respiratory infections, particularly during childhood.
Symptoms of COPD
The symptoms of COPD can vary in severity and may worsen over time. The common signs include persistent cough (with or without mucus), wheezing, shortness of breath (especially during physical exertion), chest tightness or discomfort, recurrent respiratory infections, lack of energy, unintended weight loss, and swelling in the ankles, feet, or legs. It is essential to recognize these symptoms early on and seek medical attention for proper diagnosis and treatment.
Diagnosing COPD
Medical history and physical examination
To diagnose COPD, a healthcare professional will begin by taking a detailed medical history, including any symptoms, exposure to risk factors (such as smoking or pollutants), and family history of lung diseases. A comprehensive physical examination, focusing on the lungs and respiratory system, will also be conducted. This assessment helps in ruling out other possible conditions and understanding the patient’s overall health status.
Lung function tests
Lung function tests are crucial in diagnosing COPD and determining the severity of the disease. The most common lung function test is called spirometry, which measures the amount of air you can forcefully exhale and how quickly you can do it. This test helps to assess the airflow limitation and confirm the presence of COPD. Other tests, such as lung volume measurement and gas diffusion capacity, may also be conducted to provide more detailed information about lung function.
Chest X-ray or CT scan
Chest X-rays or CT scans may be ordered to examine the structure of the lungs and rule out other lung conditions. These imaging tests help identify any abnormalities, such as lung infections, tumors, or structural lung diseases, that may be contributing to the respiratory symptoms.
Arterial blood gas test
An arterial blood gas test measures the levels of oxygen and carbon dioxide in your blood. It helps determine the severity of the COPD and assess the effectiveness of lung function. This test also provides valuable information about your body’s ability to maintain an adequate oxygen supply.
Treatments for COPD
Medications
Medications are a cornerstone of COPD treatment. They aim to improve symptoms, reduce exacerbations, and enhance overall lung function. Bronchodilators, which include both short-acting and long-acting inhalers, help relax the muscles around the airways and open them up, allowing for easier breathing. Inhaled corticosteroids may be prescribed in combination with bronchodilators to reduce inflammation and mucus production. Other medications, such as antibiotics and mucolytics, may be used to treat respiratory infections and thin mucus, respectively.
Supplemental oxygen therapy
Supplemental oxygen therapy may be prescribed for individuals with severe COPD who have low oxygen levels in their blood. It involves providing extra oxygen through a portable device to improve oxygenation and relieve symptoms. This therapy can enhance exercise capacity, improve sleep, and prolong survival in certain cases.
Pulmonary rehabilitation
Pulmonary rehabilitation is a comprehensive program that combines supervised exercise, education, and support to improve the quality of life for people with COPD. It aims to increase exercise tolerance, strengthen muscles, and teach breathing techniques to optimize lung function. The program is typically customized based on individual needs and may involve a multidisciplinary team of healthcare professionals, including respiratory therapists, physiotherapists, and dietitians.
Lifestyle changes
Making certain lifestyle changes is crucial in managing COPD. Quitting smoking is the most important step one can take to slow down the progression of the disease and improve overall health. Avoiding exposure to secondhand smoke and reducing exposure to environmental irritants, such as air pollution and occupational hazards, is equally important. Maintaining a healthy diet, staying physically active within one’s limits, and getting enough restful sleep are also beneficial for managing COPD.
Surgery
In some cases, surgery may be recommended for advanced COPD. Surgical interventions, such as lung volume reduction surgery or lung transplantation, aim to improve lung function and quality of life for eligible individuals. These procedures are reserved for carefully selected patients who have severe symptoms and do not respond adequately to other treatments.
Managing COPD
Developing a comprehensive treatment plan
Managing COPD requires a comprehensive treatment plan that addresses not only the immediate symptoms but also long-term goals. This plan is typically developed in collaboration with healthcare providers and may include medications, oxygen therapy, pulmonary rehabilitation, and lifestyle modifications. It is important to communicate openly with healthcare providers, discuss treatment goals, and seek their guidance for optimal management.
Monitoring and managing symptoms
Regular monitoring of symptoms is essential to ensure any changes or exacerbations are addressed promptly. Keeping track of symptoms, such as cough, shortness of breath, or increased mucus production, can help identify triggers or patterns that worsen the condition. Managing symptoms may involve adjusting medications, seeking medical advice during exacerbations, and adopting techniques to improve breathing, such as pursed-lip breathing.
Quitting smoking
Quitting smoking is the single most effective measure to slow down the progression of COPD and reduce complications. It is essential to seek support and implement strategies to quit smoking successfully. Healthcare providers can offer counseling, recommend nicotine replacement therapies or medications, or refer individuals to specialized smoking cessation programs. The sooner smoking is stopped, the greater the benefits in terms of symptom relief and improved lung health.
Vaccinations
Getting vaccinated against respiratory infections is crucial for people with COPD. Annual flu shots are recommended to protect against seasonal influenza, which can cause severe respiratory complications in individuals with compromised lung function. Additionally, the pneumonia vaccine (pneumococcal vaccine) can help prevent bacterial pneumonia, a common infection that can be life-threatening for people with COPD.
Exercise and physical activity
Although physical activity may seem challenging with COPD, regular exercise is highly beneficial. Engaging in a supervised exercise program, such as pulmonary rehabilitation, can improve exercise tolerance, build muscle strength, and enhance overall fitness. It is essential to consult healthcare providers or respiratory therapists to develop an exercise plan tailored to individual capabilities and limitations.
Avoiding triggers and irritants
Identifying and avoiding triggers and irritants that worsen COPD symptoms is essential for effective management. Common triggers include air pollution, dust, pollen, strong smells, and certain chemicals. Taking preventive measures, such as using air purifiers, wearing a mask in polluted environments, and avoiding exposure to respiratory irritants, can significantly reduce symptom flare-ups and improve overall well-being.

Living with COPD
Coping with emotional and psychological impact
Living with COPD can have a significant emotional and psychological impact on individuals. COPD may lead to feelings of anxiety, depression, and frustration due to the limitations imposed by the disease. It is crucial to acknowledge these emotional challenges and seek support from loved ones, healthcare providers, or mental health professionals. Engaging in stress management techniques, such as deep breathing exercises, meditation, or counseling, can help individuals cope with these emotional burdens.
Support groups and counseling
Support groups and counseling can provide valuable support and guidance to individuals with COPD. Connecting with others who are going through similar experiences can help lessen feelings of isolation and provide a platform for sharing coping strategies and insights. Support groups may be organized by local healthcare facilities, community organizations, or online platforms. Additionally, individual counseling or therapy sessions can offer personalized support to address specific emotional or psychological concerns.
Making adjustments to daily living
Living with COPD often requires certain adjustments to daily routines and activities. It is important to pace yourself and prioritize tasks to conserve energy and minimize breathlessness. Planning ahead for outings or travel, using assistive devices (such as portable oxygen concentrators), and seeking help with physically demanding tasks can make daily life more manageable. Taking frequent rest breaks and employing energy-saving techniques, such as sitting during showering or meal preparation, can also ease the strain on breathing.
Communication with healthcare providers
Open and effective communication with healthcare providers is crucial for optimal COPD management. Regular check-ups and follow-up appointments allow healthcare providers to monitor the disease’s progression, adjust treatment plans if necessary, and address any concerns or questions. Sharing symptoms, medication side effects, or changes in overall well-being with healthcare providers helps in providing appropriate guidance and support.
Maintaining a healthy lifestyle
Maintaining a healthy lifestyle is key to managing COPD and improving overall well-being. This includes following a balanced diet, staying hydrated, and getting enough restful sleep. Eating nutrient-rich foods, such as fruits, vegetables, whole grains, and lean proteins, can provide the necessary energy and support the immune system. Adequate hydration helps thin mucus and prevent dehydration, while proper sleep promotes the body’s healing and recovery processes.
Can a Person with COPD Get Better?
Improving lung function
While COPD is a chronic condition that cannot be fully reversed, lifestyle modifications and appropriate treatment can help improve lung function to some extent. Quitting smoking, adhering to prescribed medications, and engaging in regular exercise can slow down the decline in lung function and enhance overall respiratory health. Following an individualized treatment plan, as recommended by healthcare providers, can significantly contribute to improving lung function and reducing symptoms.
Managing symptoms and reducing exacerbations
Effective management of COPD focuses on controlling symptoms and preventing exacerbations. With proper treatment, symptom relief, such as reduced coughing, wheezing, and shortness of breath, can be achieved. Managing symptoms often involves using bronchodilators, inhaled corticosteroids, and supplemental oxygen as necessary. Avoiding triggers, such as respiratory irritants or respiratory infections, and maintaining good respiratory hygiene are also key in minimizing exacerbations.
Enhancing overall quality of life
Although COPD poses challenges, it is possible to enhance overall quality of life with the disease. Adapting to lifestyle changes, actively managing symptoms, and engaging in pulmonary rehabilitation or support groups can improve physical and emotional well-being. By integrating various treatment approaches, practicing self-care, and seeking appropriate support, individuals with COPD can lead fulfilling lives and maintain their independence to the best extent possible.
In conclusion, COPD is a chronic lung disease that requires ongoing management. Early diagnosis, adherence to treatment plans, and lifestyle modifications are vital in improving lung function, managing symptoms, and enhancing overall quality of life for individuals with COPD. By working closely with healthcare providers, making necessary adjustments, and prioritizing self-care, it is possible to maintain a fulfilling and healthy lifestyle despite the challenges posed by COPD.










