
If you or someone you know is living with asthma, you’ll understand the importance of staying informed about the latest developments in treatment. With so many advancements in medical technology happening every day, it’s crucial to know if there are any new approaches that could potentially change the way asthma is managed. From innovative inhalers to promising medications, this article will explore the exciting world of asthma treatment and keep you up to date on the latest advancements that could make a positive difference in your life.
Biologics
Introduction to biologics
Biologics are a relatively new class of medications that have proven to be effective in the treatment of various chronic diseases, including asthma. Unlike traditional medications, such as inhalers, which primarily target the symptoms of asthma, biologics work by targeting specific molecules and pathways in the immune system that are involved in the inflammatory response seen in asthma.
How biologics work in asthma treatment
In asthma, the immune system reacts to certain triggers, such as allergens or irritants, and this immune response leads to inflammation in the airways. Biologics work by blocking or inhibiting specific molecules, such as interleukins or immunoglobulins, which are responsible for triggering and sustaining this inflammatory response. By doing so, biologics help to reduce airway inflammation and subsequently improve asthma symptoms.
Types of biologics
There are several types of biologics available for the treatment of asthma, each targeting different molecules or pathways in the immune system. Some commonly used biologics include omalizumab, mepolizumab, and dupilumab. Each of these biologics has its own mechanism of action and specific indications.
Effectiveness and side effects
Biologics have shown great effectiveness in managing asthma symptoms, particularly for people with severe and uncontrolled asthma. Studies have demonstrated significant improvements in lung function, reduced exacerbations, and decreased dependence on other asthma medications in patients treated with biologics. However, as with any medication, there are potential side effects associated with the use of biologics, including injection site reactions, allergic reactions, and an increased risk of infection. It is important to discuss the potential benefits and risks of biologics with your healthcare provider.
Who can benefit from biologics
Biologics are typically recommended for patients with severe, uncontrolled asthma who have not adequately responded to other asthma medications. Your healthcare provider will assess your symptoms, asthma control, and medical history to determine if you may be a candidate for biologic treatment. It’s important to note that biologics are not suitable for everyone, and the decision to initiate biologic therapy should be made in consultation with your healthcare provider.
Targeted therapies
Overview of targeted therapies
Targeted therapies in the treatment of asthma involve the use of medications that specifically target certain pathways or molecules involved in the development and progression of asthma. These therapies aim to provide more precise and individualized treatment options for patients by directly addressing the underlying mechanisms of the disease.
Specific targets in asthma treatment
There are various targets in asthma treatment that can be addressed by targeted therapies. Some examples include blocking specific receptors involved in the inflammatory response, inhibiting certain enzymes that play a role in airway constriction, or modulating the activity of cytokines involved in immune response regulation. By targeting these specific pathways or molecules, targeted therapies can help to reduce inflammation, bronchoconstriction, and other asthma symptoms.
New drugs under development
Research and development in the field of targeted therapies for asthma are ongoing, and several new drugs are currently under investigation. These drugs target different pathways and mechanisms in asthma, such as inhibiting specific kinases involved in asthma-related inflammation or modulating certain immune cells responsible for allergic responses. While these drugs are still in the experimental stage, they hold promising potential for future asthma treatment options.
Effectiveness and limitations
Targeted therapies have shown promising results in clinical trials, with some patients experiencing significant improvements in asthma symptoms and lung function. However, it is important to note that targeted therapies may not be effective or suitable for all patients, as asthma is a complex and heterogeneous disease. Additionally, the cost and availability of targeted therapies can present limitations for some individuals. Further research and clinical trials are needed to better understand the effectiveness and long-term outcomes of targeted therapies in asthma treatment.

Precision medicine
Understanding precision medicine
Precision medicine is an approach to healthcare that takes into account individual variability in genes, environment, and lifestyle when developing treatment plans. In the context of asthma, precision medicine aims to provide personalized treatment options based on a patient’s unique genetic makeup, environmental exposures, and other relevant factors.
Personalized treatment approach using genomics
Genomics plays a significant role in precision medicine for asthma. Through the use of genetic testing, healthcare providers can identify specific genetic variants or markers that may influence a patient’s response to certain medications or their risk of developing severe asthma. This information can then be used to guide treatment decisions, such as selecting the most appropriate medications or identifying potential treatment targets.
Potential benefits for asthma patients
The use of precision medicine in asthma treatment can offer several potential benefits for patients. By tailoring treatment plans to individual characteristics, healthcare providers may be able to optimize asthma management, improve symptom control, and reduce the risk of exacerbations. Additionally, precision medicine may help identify individuals who are more likely to benefit from certain therapies, avoiding unnecessary treatments and reducing the burden of side effects.
Considerations and challenges in implementing precision medicine
While precision medicine holds great promise in the field of asthma treatment, there are several considerations and challenges that need to be addressed for its successful implementation. The accessibility and affordability of genetic testing, as well as the interpretation and integration of genetic information into clinical practice, are areas that require further development. Additionally, ethical considerations, patient privacy, and the potential for disparities in access to precision medicine should be carefully evaluated.
Digital health tools
Introduction to digital health tools
Digital health tools, such as mobile apps and wearable devices, have gained popularity in recent years as aids in managing various health conditions, including asthma. These tools leverage technology to provide patients with tools to monitor and track their symptoms, medications, and other relevant health information.
Use of mobile apps and wearable devices
Mobile apps and wearable devices can be used in asthma management to track symptoms, monitor medication adherence, and provide education and information about asthma. Some apps even allow patients to record and share their asthma triggers, allowing for better identification and avoidance of these triggers. Wearable devices, such as smart inhalers, can provide real-time data on medication usage and inhalation technique, allowing patients to better understand and optimize their inhaler use.
Benefits for asthma management
Digital health tools offer several benefits for asthma management. By providing real-time symptom tracking and medication reminders, these tools can help patients stay engaged in their treatment plan and adhere to their prescribed medications. The ability to monitor triggers and identify patterns in symptom exacerbations can also aid in personalized asthma management. Additionally, digital health tools can facilitate remote monitoring and communication between patients and healthcare providers, enhancing the overall management of asthma.
Limitations and concerns
While digital health tools have shown promise in improving asthma management, there are some limitations and concerns that need to be considered. Not all individuals may have access to the necessary technology or may not feel comfortable using digital tools. Additionally, the accuracy and reliability of some apps and devices have raised concerns. It is important for patients to discuss the use of digital health tools with their healthcare provider to ensure their appropriateness and effectiveness in their specific asthma management plan.
Immunotherapy
Overview of immunotherapy
Immunotherapy, also known as allergy shots or desensitization, is a treatment approach that involves introducing small amounts of allergens into the body in order to reduce the immune system’s response to these allergens. Immunotherapy has been used for many years to treat allergic rhinitis and has also shown effectiveness in managing asthma triggered by allergies.
Subcutaneous immunotherapy (SCIT)
Subcutaneous immunotherapy involves the administration of allergens via injections under the skin. Initially, small doses are given, and the dosage gradually increases over time. The goal is to desensitize the immune system to the allergens, reducing the severity of the allergic response and subsequently reducing asthma symptoms triggered by allergies. This form of immunotherapy requires regular visits to a healthcare provider for the administration of the injections.
Sublingual immunotherapy (SLIT)
Sublingual immunotherapy involves the administration of allergens in the form of drops or tablets under the tongue. These allergens are absorbed through the sublingual mucosa, desensitizing the immune system in a similar manner to subcutaneous immunotherapy. SLIT is generally more convenient and can be self-administered at home, but it may take longer to achieve the desired therapeutic effect compared to subcutaneous immunotherapy.
Effectiveness and considerations for asthma treatment
Immunotherapy has been shown to be effective in reducing asthma symptoms and medication use in individuals with allergic asthma. It can also help to improve asthma control and reduce the risk of exacerbations triggered by allergens. However, immunotherapy is typically recommended for individuals with allergic asthma who have well-documented allergen sensitivities. It may not be suitable for everyone, and the decision to pursue immunotherapy should be made in consultation with a healthcare provider.
Lung remodeling treatments
Understanding lung remodeling in asthma
Lung remodeling refers to the structural changes that occur in the airways of individuals with asthma. Chronic inflammation and repeated episodes of bronchoconstriction can lead to the remodeling of the airway walls, resulting in thickening of the smooth muscle, increased vascularization, and deposition of extracellular matrix proteins. These structural changes can contribute to the persistent airflow limitation and symptoms seen in asthma.
Emerging treatments targeting lung remodeling
Several emerging treatments are being investigated for their potential to target and reverse lung remodeling in asthma. These treatments aim to modify the underlying structural changes in the airways, potentially leading to improved lung function and symptom control. Examples of emerging treatments include monoclonal antibodies targeting specific pathways involved in airway remodeling and novel pharmacological agents that inhibit the synthesis or deposition of extracellular matrix proteins.
Potential benefits for asthma patients
If successful, lung remodeling treatments could provide significant benefits for individuals with asthma. By targeting the underlying structural changes in the airways, these treatments may help to improve lung function, reduce symptoms, and enhance asthma control. They have the potential to offer a more comprehensive approach to asthma management, targeting not only the inflammation but also the structural changes that contribute to the disease.
Research and development in this field
Research and development in the field of lung remodeling treatments are ongoing, with scientists and healthcare providers actively exploring various strategies and interventions. Clinical trials are being conducted to evaluate the safety and effectiveness of these emerging treatments, and the results are anticipated in the coming years. Continued advancements in understanding the mechanisms of lung remodeling in asthma will likely lead to novel and more targeted therapeutic approaches in the future.
Novel inhaler technologies
Advancements in inhaler devices
Inhaler devices have evolved significantly over the years, and there have been several advancements in the design and functionality of these devices. Traditional pressurized metered-dose inhalers (MDIs) have been refined and improved, and novel types of inhalers, such as dry powder inhalers (DPIs) and soft mist inhalers (SMIs), have been developed.
Smart inhalers and their benefits
Smart inhalers are a type of inhaler device that incorporates digital technology to provide additional features and benefits for asthma management. These devices can track and record medication usage, monitor inhalation technique, and provide reminders for medication administration. Smart inhalers can also transmit data to healthcare providers or mobile apps, allowing for remote monitoring and greater insight into an individual’s asthma management.
Improving medication adherence
One of the key advantages of novel inhaler technologies, including smart inhalers, is their potential to improve medication adherence. By providing reminders and tracking medication usage, these devices can help individuals stay on track with their prescribed therapies. Improved adherence can lead to better asthma control and reduced risk of exacerbations.
Enhanced drug delivery mechanisms
Novel inhaler technologies also offer the potential for enhanced drug delivery mechanisms. DPIs, for example, have been shown to improve the lung deposition of medications compared to traditional MDIs. SMIs, on the other hand, generate a fine mist that can reach deeper into the lungs, improving drug delivery to the targeted areas. These advancements in drug delivery technology can result in more efficient and effective management of asthma symptoms.
Self-management strategies
Patient education and self-care
Patient education and self-care are crucial components of asthma management. By providing individuals with the knowledge and skills to understand and control their asthma, they can take an active role in managing their condition. Patient education may include information on asthma triggers, proper inhaler technique, identifying early warning signs of an asthma attack, and the importance of adhering to prescribed medications.
Developing an asthma action plan
An asthma action plan is a personalized document that outlines strategies for managing asthma symptoms and exacerbations. It typically includes information on daily asthma management, such as medication usage and symptom monitoring, as well as instructions on what to do in the event of worsening symptoms or an asthma attack. An asthma action plan helps individuals take timely and appropriate actions to prevent or manage asthma exacerbations effectively.
Monitoring symptoms and triggers
Regular monitoring of asthma symptoms and identification of triggers can help individuals better understand their condition and take appropriate actions to manage it. Keeping a symptom diary or using mobile apps to track symptoms and potential triggers can provide valuable information for both the individuals and their healthcare providers. By identifying patterns and triggers, individuals can make informed decisions about lifestyle modifications and avoid exposure to allergens or irritants that may worsen their asthma symptoms.
Benefits of self-management
Self-management strategies in asthma can provide numerous benefits for individuals with the condition. By actively participating in their own care and following a well-defined asthma action plan, individuals can achieve better asthma control, reduce the risk of exacerbations, and improve their quality of life. Self-management empowers individuals to take control of their asthma and make informed decisions about their treatment and lifestyle choices.

Alternative therapies
Overview of alternative therapies
Alternative therapies are non-conventional approaches to healthcare that are used in addition to or instead of traditional medical treatments. In the context of asthma, some individuals may explore alternative therapies as a complementary approach to manage their symptoms or as an alternative to conventional asthma medications.
Acupuncture and acupressure
Acupuncture and acupressure are practices rooted in Chinese traditional medicine that involve the insertion of thin needles or the application of pressure to specific points on the body. Some individuals with asthma have reported symptom relief and improved lung function following acupuncture or acupressure treatments. However, the scientific evidence supporting these practices in asthma management is limited, and more research is needed to determine their effectiveness.
Herbal remedies and supplements
Herbal remedies and supplements are another category of alternative therapies that are sometimes used in asthma management. Some herbs, such as Boswellia serrata and ginger, have been traditionally used for their anti-inflammatory properties and have been studied for their potential benefits in managing asthma symptoms. However, it is important to note that the safety, efficacy, and potential interactions of herbal remedies and supplements with conventional asthma medications are not well-established. Consultation with a healthcare provider is crucial before considering the use of any herbs or supplements in asthma management.
Evidence and considerations
While alternative therapies may offer a more holistic approach to healthcare, it is important to approach them with caution and critical thinking. The evidence supporting the effectiveness of alternative therapies in asthma management is often limited and mixed. Additionally, the use of alternative therapies should not replace or delay seeking appropriate medical care for asthma. It is essential to discuss the use of alternative therapies with a healthcare provider to ensure their safety, appropriateness, and potential interactions with conventional asthma treatments.
Combination therapies
Benefits of combining different asthma medications
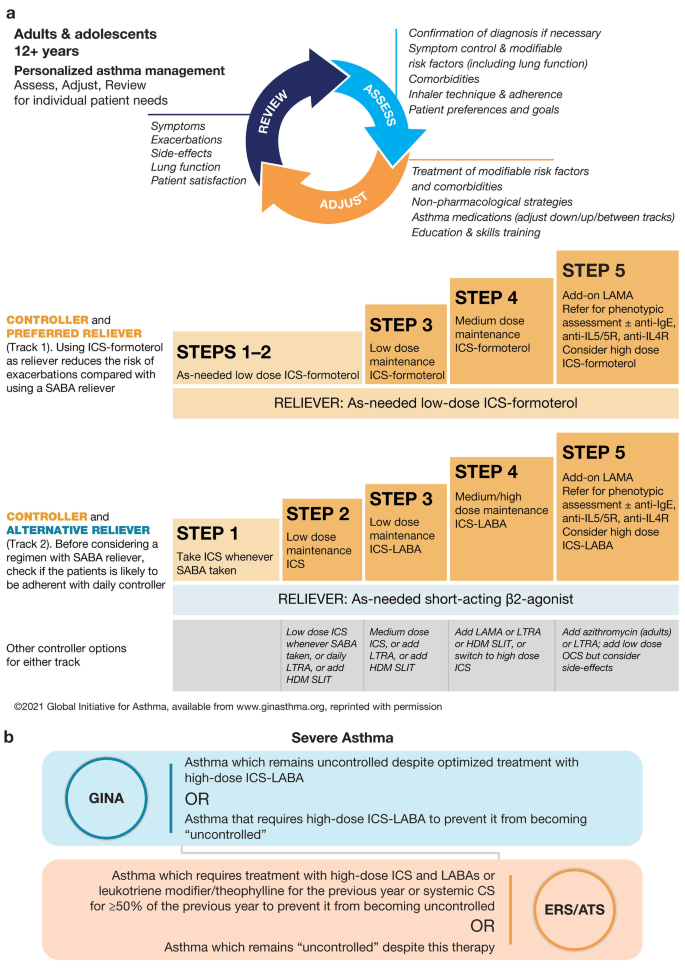
Combination therapies involve the use of multiple asthma medications with different mechanisms of action to achieve better symptom control and asthma management. By combining medications that target different aspects of asthma, such as inflammation and bronchoconstriction, healthcare providers can optimize treatment outcomes and improve overall asthma control. Combination therapies can be particularly beneficial for individuals with moderate to severe asthma or those who have not adequately responded to monotherapy.
Commonly used combinations
Some commonly used combinations of asthma medications include inhaled corticosteroids combined with long-acting beta-agonists (LABAs), which provide both anti-inflammatory and bronchodilator effects. Other combinations may include a biologic medication along with standard maintenance therapy. These combinations are tailored to the individual needs of the patient and are prescribed based on the severity and characteristics of their asthma.
Emerging combination therapies
Research and development in the field of combination therapies for asthma are ongoing, and new combinations of medications are being explored. For example, combining two biologic medications with different targets in the immune system may provide additional benefits for individuals with severe asthma. The efficacy and safety of these emerging combination therapies are being investigated in clinical trials, and their potential role in asthma management is yet to be fully determined.
Effectiveness and considerations
Combination therapies have shown to be effective in improving asthma control and reducing symptoms in individuals with moderate to severe asthma. They offer the advantage of targeting multiple aspects of the disease, providing more comprehensive management. However, it is important to consider the potential side effects and medication interactions associated with combination therapies. Regular monitoring and communication with a healthcare provider are essential to ensure the effectiveness and safety of combination therapies in individual patients.










